Chapter: Clinical Anesthesiology: Clinical Pharmacology: Intravenous Anesthetics
Intravenous Anesthetics: Etomidate
ETOMIDATE
Mechanisms of Action
Etomidate depresses the reticular
activating system and mimics the inhibitory effects of GABA. Specifi-cally,
etomidate—particularly the R(+) isomer— appears to bind to a subunit
of the GABAA receptor, increasing the receptor’s
affinity for GABA. Unlike barbiturates, etomidate may have disinhibitory
effects on the parts of the nervous system that control extrapyramidal motor
activity. This disinhi-bition offers a potential explanation for the 30–60%
incidence of myoclonus with etomidate induction ofanesthesia.
Structure–Activity Relationships
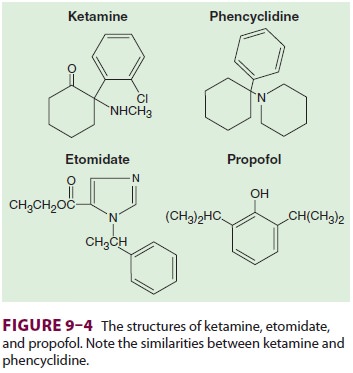
Etomidate contains a carboxylated
imidazole and is structurally unrelated to other anesthetic agents (see Figure
9–4). The imidazole ring provides water solubility in acidic solutions and
lipid solubility at physiological pH. Therefore etomidate is dissolved in
propylene glycol for injection. This solution often causes pain on injection
that can be lessened by a prior intravenous injection of lidocaine.
Pharmacokinetics
A. Absorption
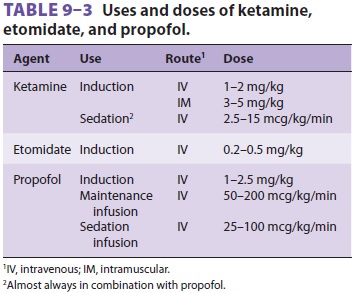
Etomidate is available only for
intravenous admin-istration and is used primarily for induction of gen-eral
anesthesia (see Table 9–3). It is sometimes used for brief production of deep
(unconscious) sedation such as prior to placement of retrobulbar blocks.
B. Distribution
Although it is highly protein bound,
etomidate is characterized by a very rapid onset of action due to its great
lipid solubility and large nonionized fraction at physiological pH.
Redistribution is responsible for decreasing the plasma concentration to
awakening levels. Etomidate plasma kinetics are well explained by a
two-compartment model.
C. Biotransformation
Hepatic microsomal enzymes and plasma
esterases rapidly hydrolyze etomidate to an inactive metabolite.
D. Excretion
The end products of etomidate hydrolysis
are pri-marily excreted in the urine.
Effects on Organ Systems
A. Cardiovascular
Etomidate has minimal effects on the
cardiovascu-lar system. A mild reduction in peripheral vascular resistance is
responsible for a slight decline in arterial blood pressure. Myocardial
contractility and cardiac output are usually unchanged. Etomidate does not
release histamine. However, etomidate by itself, even in large doses, produces
relatively light anesthesia for laryngoscopy, and marked increases in heart
rate and blood pressure may be recorded when etomidate provides the only
anesthetic depth for intubation.
B. Respiratory
Ventilation is affected less with
etomidate than with barbiturates or benzodiazepines. Even induction doses
usually do not result in apnea unless opioids have also been administered.
C. Cerebral
Etomidate decreases cerebral metabolic
rate, cere-bral blood flow, and intracranial pressure. Because of minimal
cardiovascular effects, CPP is well main-tained. Although changes on EEG
resemble those associated with barbiturates, etomidate increases the amplitude
of somatosensory evoked potentials. Postoperative nausea and vomiting are more
com-mon following etomidate than following propofol or barbiturate induction.
Etomidate lacks analgesic properties.
D. Endocrine
Induction doses of etomidate transiently
inhibit enzymes involved in cortisol and aldosterone synthesis. It was used in
the past for sedation in the intensive care unit (ICU) before reports of its
consistent ability to produce adrenocortical suppression in that circumstance
appeared. Long-term infusion and adrenocortical
suppression were associated with an increased mortality rate in critically
ill (particularly septic) patients.
Drug Interactions
Fentanyl increases the plasma level and
prolongs the elimination half-life of etomidate. Opioids decrease the myoclonus
characteristic of an etomi-date induction.
Related Topics