Chapter: Clinical Anesthesiology: Clinical Pharmacology: Intravenous Anesthetics
Intravenous Anesthetics: Benzodiazepines
BENZODIAZEPINES
Mechanisms of Action
Benzodiazepines bind the same set of
receptors in the central nervous system as barbiturates but bind to a different
site on the receptors. Benzodiazepine binding to the GABAA receptor increases the fre-quency of openings of
the associated chloride ion channel. For example, benzodiazepine-receptor
binding facilitates binding of GABA to its receptor. Flumazenil (an imidazobenzodiazepine) is a spe-cific
benzodiazepine–receptor antagonist that effec-tively reverses most of the
central nervous system effects of benzodiazepines .
Structure–Activity Relationships
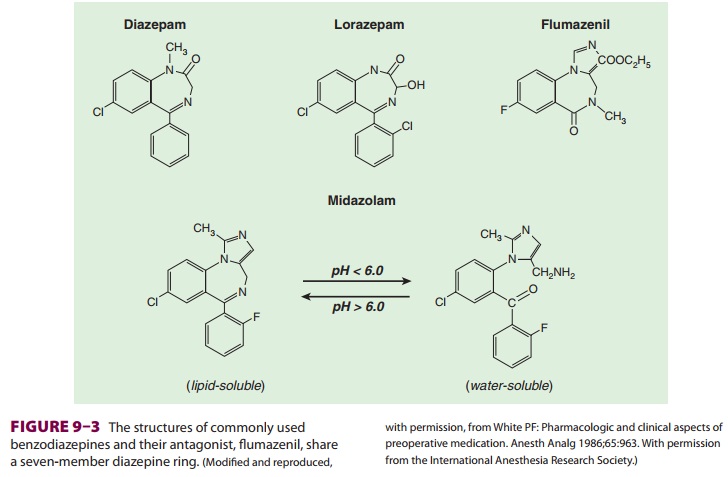
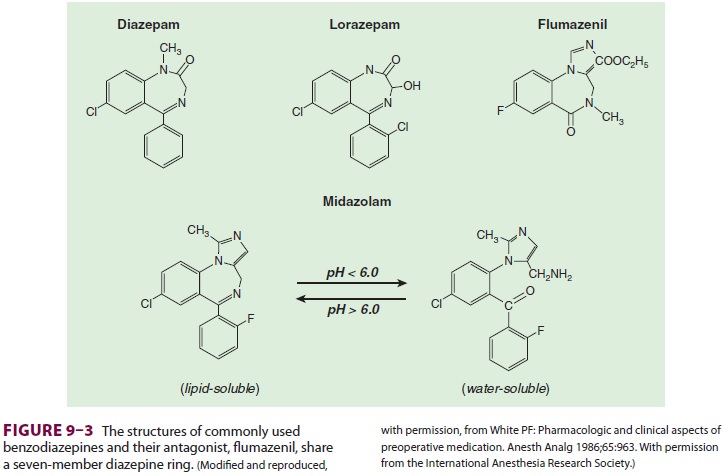
The chemical structure of
benzodiazepines includes a benzene ring and a seven-member diazepine ring (Figure 9–3).
Substitutions at various positions on these rings affect potency and
biotransformation. The imidazole ring of midazolam contributes to its water
solubility at low pH. Diazepam and lorazepam are insoluble in water so
parenteral preparations contain propylene glycol, which can produce venous
irritation.
Pharmacokinetics
A. Absorption
Benzodiazepines are commonly
administered orally, intramuscularly, and intravenously to provide seda-tion
or, less commonly, to induce general anesthe-sia (Table 9–2). Diazepam and
lorazepam are well absorbed from the gastrointestinal tract, with peak plasma
levels usually achieved in 1 and 2 h, respec-tively. Oral midazolam has not
been approved by the U.S. Food and Drug Administration, nevertheless this route
of administration has been popular for pediatric premedication. Likewise,
intranasal (0.2– 0.3 mg/kg), buccal (0.07 mg/kg), and sublingual (0.1 mg/kg)
midazolam provide effective preoperative sedation.
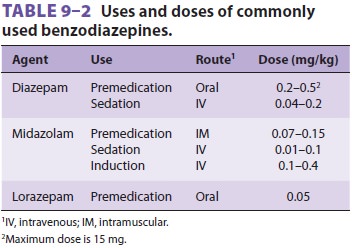
Intramuscular injections of diazepam are pain-ful and unreliably absorbed. In contrast, midazolam and lorazepam are well absorbed after intramuscu-lar injection, with peak levels achieved in 30 and 90 min, respectively. Induction of general anesthesia with midazolam is convenient only with intravenous administration.
B. Distribution
Diazepam is relatively lipid soluble and
readily penetrates the blood–brain barrier. Although mid-azolam is water
soluble at reduced pH, its imidaz-ole ring closes at physiological pH,
increasing its lipid solubility (see Figure 9–3). The moderate lipid solubility
of lorazepam accounts for its slower brain uptake and onset of action.
Redistribution is fairly rapid for the benzodiazepines (the initial
distribu-tion half-life is 3–10 min) and, like the barbiturates, is responsible
for awakening. Although midazolam has been used as an induction agent, neither
mid-azolam nor any other of the benzodiazepines can match the rapid onset and
short duration of action of propofol or even thiopental. All three benzodiaz-epines
are highly protein bound (90–98%).
C. Biotransformation
The benzodiazepines rely on the liver
for biotrans-formation into water-soluble glucuronidated end products. The
phase I metabolites of diazepam are pharmacologically active.Slow hepatic
extraction and a large volume of distribution (Vd) result in a long elimination half-life
for diazepam (30 h). Although lorazepam also has a low hepatic extraction
ratio, its lower lipid solubility limits its Vd, resulting in a shorter elimination
half-life (15 h). Nonetheless, the clini-cal duration of lorazepam is often
quite prolonged due to increased receptor affinity. These differ-ences between
lorazepam and diazepam illustrate the low utility of individual pharmacokinetic
half-lives in guiding clinical practice. Midazolam shares diazepam’s Vd,
but its elimination half-life (2 h) is the shortest of the group because of its
increased hepatic extraction ratio.
D. Excretion
The metabolites of benzodiazepine
biotransforma-tion are excreted chiefly in the urine. Enterohepatic circulation
produces a secondary peak in diazepam plasma concentration 6–12 h following
administra-tion. Kidney failure may lead to prolonged seda-tion in patients
receiving larger doses of midazolam due to the accumulation of a conjugated
metabolite (α-hydroxymidazolam).
Effects on Organ Systems
A. Cardiovascular
The benzodiazepines display minimal
cardiovascular depressant effects even at general anesthetic doses, except when
they are coadministered with opioids (these agents interact to produce
myocardial depres-sion and arterial hypotension). Benzodiazepines given alone
decrease arterial blood pressure, cardiac output, and peripheral vascular
resistance slightly, and sometimes increase heart rate. Intravenous mid-azolam
tends to reduce blood pressure and peripheral vascular resistance more than
diazepam. Changes in heart rate variability during midazolam sedation sug-gest
decreased vagal tone (ie, drug-induced vagolysis).
B. Respiratory
Benzodiazepines depress the ventilatory
response to CO2. This depression is usually
insignificant unless the drugs are administered intravenously or in
asso-ciation with other respiratory depressants. Although apnea may be
relatively uncommon after ben-zodiazepine induction, even small intravenous
doses of diazepam and midazolam have resulted in respiratory arrest. The steep
dose–response curve, slightly prolonged onset (compared with propofol or
thiopental), and potency of midazolam necessitate careful titration to avoid
overdosage and apnea. Ventilation must be monitored in all patients receiv-ing
intravenous benzodiazepines, and resuscitation equipment must be immediately
available.
C. Cerebral
Benzodiazepines reduce cerebral oxygen
consump-tion, cerebral blood flow, and intracranial pressure but not to the
extent the barbiturates do. They are effective in preventing and controlling
grand mal seizures. Oral sedative doses often produce ante-grade amnesia, a
useful premedication property. The mild muscle-relaxing property of these drugs
is mediated at the spinal cord level, not at the neu-romuscular junction. The
antianxiety, amnestic, and sedative effects seen at lower doses progress to
stupor and unconsciousness at induction doses. Compared with propofol or
thiopental, induction with benzodiazepines is associated with a slower rate of
loss of consciousness and a longer recovery. Benzodiazepines have no direct
analgesic properties.
Drug Interactions
Cimetidine binds to cytochrome P-450 and
reduces the metabolism of diazepam. Erythromycin inhib-its metabolism of
midazolam and causes a two- to threefold prolongation and intensification of
its effects. Heparin displaces diazepam from pro-tein-binding sites and
increases the free drug concentration.
As previously mentioned, the combination
of opioids and benzodiazepines markedly reduces arterial blood pressure and
peripheral vascular resis-tance. This synergistic interaction has often been
observed in patients with ischemic or valvular heart disease who often receive
benzodiazepines for pre-medication and during induction of anesthesia with
opioids.Benzodiazepines reduce the minimum alveolar concentration of volatile
anesthetics as much as 30%.Ethanol, barbiturates, and other central nervous
system depressants potentiate the sedative effects of the benzodiazepines.
Related Topics