Chapter: Obstetrics and Gynecology: Contraception
Intrauterine Contraception
INTRAUTERINE CONTRACEPTION
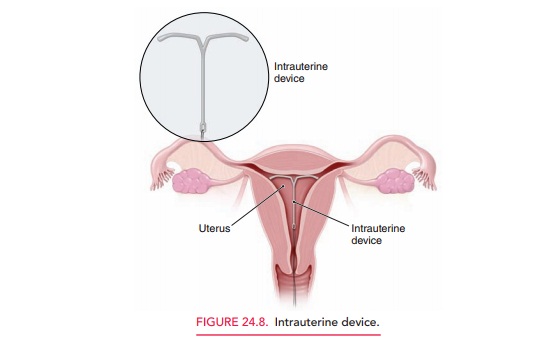
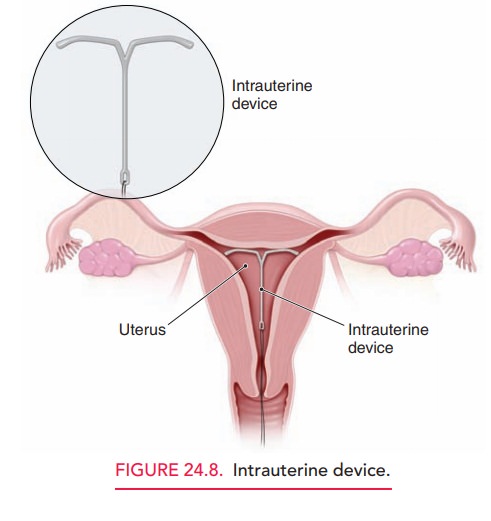
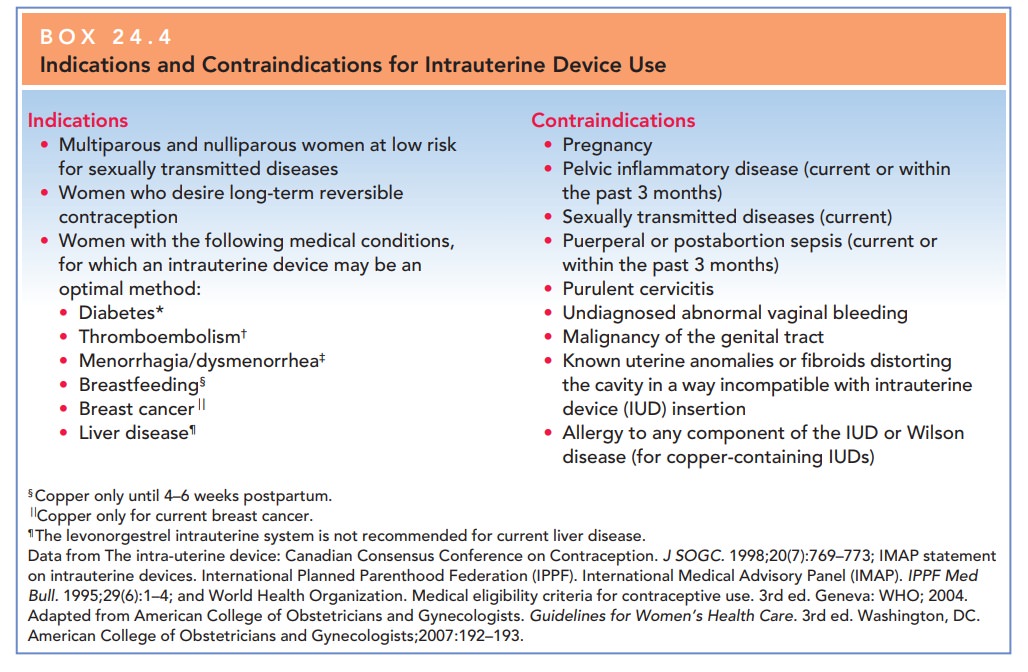
Intrauterine contraceptives, also known as intrauterine devices (IUDs), are among the most commonly usedand safe methods of interval contraception worldwide (Fig. 24.8). Two types of IUDs are available in the United States. Both are T-shaped. One releases a small amount of levonorgestrel into the uterus, and the other releases a small amount of copper into the uterus.
The Lippe loop is an unmedicated
IUD available throughout the world except in the United States. The
levonorgestrel-containing device primarily works by pre-venting the sperm and
egg from meeting. It also thick-ens the cervical mucus and creates an
unfavorable uterine environment. The copper in the copper-containing device can
prevent the egg from being fertilized or from attach-ing to the wall of the
uterus. It also prevents sperm from going into the uterus and the fallopian
tube, reducing the sperm’s ability to fertilize an egg. The copper-containing
IUD is also used postcoitally as emergency contraception.
A clinically important side
effect of the levonorgestrel-containing IUD is a decrease in menstrual blood
loss (up to 50%) and severity of dysmenorrhea. Serum proges-terone levels are
not affected. IUD removal is followed by rapid reversal of these effects and
return to a normal intrauterine environment and normal fertility. This sys-tem
is used to relieve pain related to endometriosis and ade-nomyosis as well as
for endometrial protection for women taking hormone replacement therapy who
cannot take oral progestins (Box 24.4). Increased vaginal bleeding and
menstrual pain are experienced by 5% to 10% of women and often result in their
request to discontinue IUD use.
The progestin IUDs have a lesser
incidence of this prob-lem, because of the progestin effect on the endometrium.
Bacteria from the endogenous
cervicovaginal flora can be introduced into the uterus during IUD insertion and
may cause infection. Prophylactic antibiotics have not been shown to decrease
the incidence of this type of infection. Sterile technique and a vaginal prep
with Betadine should be used prior to insertion of an IUD. Pelvic infection
oc-curring 3 or more months after IUD insertion may be pre-sumed to be an
acquired STD and treated accordingly. Women at high risk for STDs may benefit
from screen-ing prior to insertion. Asymptomatic IUD users with pos-itive
cervical cultures for gonorrhea or chlamydia, or with bacterial vaginosis,
should be treated promptly. The IUD may remain in place unless there is
evidence of spread of the infection to the endometrium or fallopian tubes and/
or failure of treatment with appropriate antibiotics.
The IUDs
presently available in the United States are highly effective. The
copper-containing IUD has a recom-mended lifespan of 10 years and demonstrates
a pregnancy rate of 0.5% to 0.8%. The levonorgestrel-releasing IUD lasts for up
to 5 years and has a pregnancy rate of 0.2%. The overall expulsion rate for
IUDs is 1% to 5%, with the greatest likelihood in the first few months of use.
Expulsion is often preceded by cramping, vaginal discharge, or bleed-ing,
although it may be asymptomatic, with the only evi-dence being the observed
lengthening of the IUD string or the partner feeling the device during intercourse.
Pa-tients should be counseled to see their clinician if expul-sion is
suspected.
The IUDs do not increase the
overall risk of ectopic pregnancy. However, because the IUD offers greater
pro-tection against intrauterine than extrauterine pregnancy, the relative
ratio of extrauterine pregnancy is greater in a woman who uses an IUD than in a
woman not using con-traception. Therefore, in the rare instance that a woman
with an IUD in place becomes pregnant, that pregnancy would have a high risk of
being extra-uterine.
About 40% to 50% of patients who
become preg-nant with an IUD in place will spontaneously abort in the first
trimester. Because of this risk, patients should be offered IUD removal if the
string is visible; this is as-sociated with a decreased spontaneous abortion
rate of about 30%. If the IUD string is not visible, instrumen-tal removal may
be performed, but the risk of pregnancy disruption is increased. If the IUD is
left in place, preg-nancy may proceed uneventfully. There is no evidence of an
increased risk of congenital anomalies with either med-icated or unmedicated
devices. There is, however, an ap-proximate twofold to fourfold increase in the
incidence of preterm labor and delivery.
Patient selection and skillful
insertion are crucial to the successful use of the IUD as a method of
contracep-tion. The risk of sexually transmitted infections is the most
important factor in patient selection, not age and parity.
IUD insertion is best
accomplished when the patient is menstruating. This timing is beneficial
because it con-firms the patient is not pregnant and her cervix is usually
slightly open. If that timing cannot be achieved, it can be done at other times
in the cycle as the patient is switching from another reliable method of
contraception. The de-vices may also be inserted in breastfeeding women, who,
in fact, demonstrate a lower incidence of postinsertional discomfort and
bleeding. All IUD insertion techniques share the same basic rules: careful
bimanual examination before insertion to determine the likely direction of
in-sertion into the endometrial cavity, proper loading of the device into the
inserter, careful placement to the fundal margin of the endometrial cavity, and
proper inserter re-moval while leaving the IUD in place.
The IUD is removed by simply
pulling on the string. If the string is not visible, rotating two cotton-tip
appli-cators in the endocervical canal will often retrieve the strings. If this
is not possible, a fine probe may be inserted, the IUD felt, and then removed
with an “IUD hook” or small forceps. If needed, ultrasound guidance can assist
in this process. Infrequently, IUDs become embedded in the uterine wall and
require hysteroscopic removal. Even less frequently, an IUD perforates the
uterus (at insertion, but is not always recognized) and requires laparoscopic
removal.
Related Topics