Chapter: Basic & Clinical Pharmacology : Agents That Affect Bone Mineral Homeostasis
Interaction of PTH, FGF23, & Vitamin D
INTERACTION OF PTH, FGF23, &
VITAMIN D
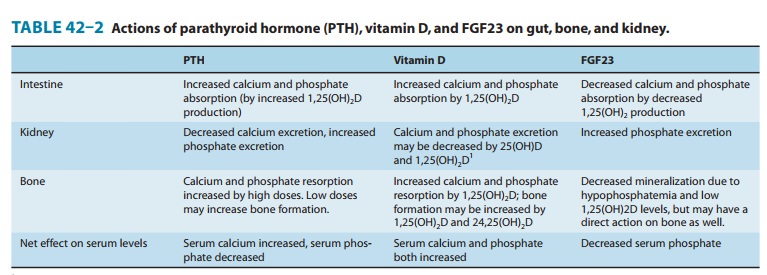
A summary of the
principal actions of PTH, FGF23, and vitamin D on the three main target
tissues—intestine, kidney, and bone—is presented in Table 42–2. The net effect
of PTH is to raise serum calcium and reduce serum phosphate; the net effect of
FGF23 is to decrease serum phosphate; the net effect of vitamin D is to raise
both. Regulation of calcium and phosphate homeostasis is achieved through
important feedback loops. Calcium is one of two principal regulators of PTH
secretion. It binds to a novel ion recognition site that is part of a Gq protein-coupled
receptor called the calcium-sensing receptor (CaSR) that employs the
phosphoinositide second messenger system to link changes in the extracellular
cal-cium concentration to changes in the intracellular free calcium. As serum
calcium levels rise and activate this receptor, intracellular calcium levels
increase and inhibit PTH secretion. This inhibi-tion by calcium of PTH secretion,
along with inhibition of renin and atrial natriuretic factor secretion, is the
opposite of the effect in other tissues such as the beta cell of the pancreas,
in which calcium stimulates secretion. Phosphate regulates PTH secretion
directly and indirectly by forming complexes with calcium in the serum. Because
it is the ionized free concentration of extracellular calcium
Such feedback regulation is
appropriate to the net effect of PTH to raise serum calcium and reduce serum
phosphate levels. Likewise, both calcium and phosphate at high levels reduce
the amount of 1,25(OH)2D produced by the kidney and increase the amount of 24,25(OH)2D produced.
High
serum calcium works directly and indirectly by reducing PTH secretion. High
serum phosphate works directly and indirectly by increasing FGF23 levels. Since
1,25(OH)2D raises serum calcium and
phosphate, whereas 24,25(OH)2D has less
effect, such feedback regulation is again appropriate. 1,25(OH)2D
directly inhibits PTH secretion (independent of its effect on serum calcium) by
a direct inhibitory effect on PTH gene transcription. This pro-vides yet
another negative feedback loop. In patients with chronic renal failure who
frequently are deficient in producing 1,25(OH)2D,
loss of this 1,25(OH)2D-mediated
feedback loop coupled with impaired phosphate excretion and intestinal calcium
absorption often leads to secondary hyperparathyroidism. The ability of
1,25(OH)2D to inhibit PTH secretion directly
is being exploited with calcitriol analogs that have less effect on serum
calcium because of their lesser effect on intestinal calcium absorption. Such
drugs are proving useful in the management of secondary hyperparathy-roidism
accompanying chronic kidney disease and may be useful in selected cases of
primary hyperparathyroidism. 1,25(OH)2D
also stimulates the production of FGF23. This completes the negative feedback
loop in that FGF23 inhibits 1,25(OH)2D
production while promoting hypophosphatemia, which in turn inhibits FGF23
production and stimulates 1,25(OH)2D
production.
Related Topics