Chapter: Essentials of Anatomy and Physiology: Lymphatic System and Immunity
Innate Immunity
INNATE IMMUNITY
Innate immunity is accomplished by physical barriers, chemical mediators, white blood cells, and the inflammatory response.
Physical Barriers
Physical barriers prevent pathogens and chemicals from enteringthe body in two ways: (1) The skin and mucous membranes form barriers that prevent their entry, and (2) tears, saliva, and urine wash these substances from body surfaces. Pathogens cannot cause a disease if they cannot get into the body.
Chemical Mediators
Chemical mediators are molecules responsible for many aspectsof innate immunity. Some chemicals on the surface of cells destroy pathogens or prevent their entry into the cells. For example, lysozyme in tears and saliva kills certain bacteria, and mucus on the mucous membranes prevents the entry of some pathogens.
Other chemical mediators, such as histamine (his′ tă-mēn), complement, prosta-glandins (pros-tă-glan′ dinz), and leukotrienes (loo-kō-trı̄′ ēnz), promote inflammation by causing vasodilation, increasing vascular permeability, and stimulating phagocytosis. In addition, interfer-ons protect cells against viral infections.
Complement
Complement (kom′ plĕ-ment) is a group of more than 20 proteinsfound in plasma. The operation of complement proteins is similar to that of clotting proteins . Normally, comple-ment proteins circulate in the blood in an inactive form. Certain complement proteins can be activated by combining with foreign substances, such as parts of a bacterial cell, or by combining with antibodies (see “Effects of Antibodies” later). Once activation begins, a series of reactions results, in which each complement protein activates the next. Once activated, certain complement proteins promote inflammation and phagocytosis and can directly lyse (rupture) bacterial cells.
Interferons
Interferons (in-ter-fēr′ onz) are proteins that protect the bodyagainst viral infections. When a virus infects a cell, the infected cell produces viral nucleic acids and proteins, which are assembled into new viruses. The new viruses are then released to infect other cells. Because infected cells usually stop their normal functions or die during viral replication, viral infections are clearly harmful to the body. Fortunately, viruses often stimulate infected cells to produce interferons, which do not protect the cell that produces them. Instead, interferons bind to the surface of neighboring cells, where they stimulate those cells to produce antiviral proteins. These antiviral proteins inhibit viral reproduction by preventing the production of new viral nucleic acids and proteins.
Some interferons play a role in activating immune cells, such as macrophages and natural killer cells (see next section).
White Blood Cells
White blood cells and the cells derived fromthem are the most important cellular components of immunity. White blood cells are produced in red bone marrow and lym-phatic tissue and released into the blood. Chemicals released from pathogens or damaged tissues attract the white blood cells, and they leave the blood and enter affected tissues. Important chemicals known to attract white blood cells include complement, leukotrienes, kinins (kı̄′ ninz), and histamine. The movement of white blood cells toward these chemicals is called chemotaxis (kem-ō-tak′ sis, kē-mō-tak′ sis).
Phagocytic Cells
Phagocytosis (fag′ ō-sı̄-tō′ sis) is the ingestion and destruction ofparticles by cellscalled phagocytes (fag′ ō-sı̄tz) . The particles can be microorganisms or their parts, foreign sub-stances, or dead cells from the body. The most important phago-cytes are neutrophils and macrophages, although other white blood cells also have limited phagocytic ability.
Neutrophils (noo′ trō-filz) are small phagocytic cells that areusually the first cells to enter infected tissues from the blood in large numbers. They release chemical signals that increase theinflammatory response by recruiting and activating other immune cells. Neutrophils often die after phagocytizing a single micro-organism. Pus is an accumulation of fluid, dead neutrophils, and other cells at a site of infection.
Macrophages (mak′ rō-fā′ jes) are monocytes that leave theblood, enter tissues, and enlarge about fivefold. Monocytes and macrophages form the mononuclear phagocytic system because they are phagocytes with a single (mono), unlobed nucleus. Sometimes macrophages are given specific names, such as dustcells in the lungs, Kupffer cells in the liver, and microglia in thecentral nervous system. Macrophages can ingest more and larger items than can neutrophils. Macrophages usually appear in infected tissues after neutrophils do, and they are responsible for most of the phagocytic activity in the late stages of an infection, including cleaning up dead neutrophils and other cellular debris.
In addition to leaving the blood in response to an infection, macrophages are also found in uninfected tissues. If pathogens enter uninfected tissue, the macrophages may phagocytize the microorganisms before they can replicate or cause damage. For example, macrophages are located at potential points where patho-gens may enter the body, such as beneath the skin and mucous membranes, and around blood and lymphatic vessels. They also protect lymph in lymph nodes and blood in the spleen and liver.
Cells of Inflammation
Basophils, which are derived from red bone marrow, are motilewhite blood cells that can leave the blood and enter infected tissues. Mast cells, which are also derived from red bone marrow, arenonmotile cells in connective tissue, especially near capillaries. Like macrophages, mast cells are located at points where pathogens may enter the body, such as the skin, lungs, gastrointestinal tract, and urogenital tract.
Basophils and mast cells can be activated through innate immunity (e.g., by complement) or through adaptive immunity (see “Adaptive Immunity” later). When activated, they release chemicals, such as histamine and leukotrienes, that produce an inflammatory response or activate other mechanisms, such as smooth muscle contraction in the lungs. Eosinophils also participate in inflammation associated with allergies and asthma.
Inflammation is beneficial in the fight against pathogens, but too much inflammation can be harmful, destroying healthy tissues as well as the microorganisms.
Natural Killer Cells
Natural killer (NK) cells, a type of lymphocyte produced in redbone marrow, account for up to 15% of lymphocytes. NK cells rec-ognize classes of cells, such as tumor cells or virus-infected cells, in general, rather than specific tumor cells or cells infected by a specific virus. For this reason, and because NK cells do not exhibit a memory response, they are classified as part of innate immunity. NK cells use a variety of methods to kill their target cells, including releasing chemicals that damage cell membranes and cause the cells to lyse.
Inflammatory Response
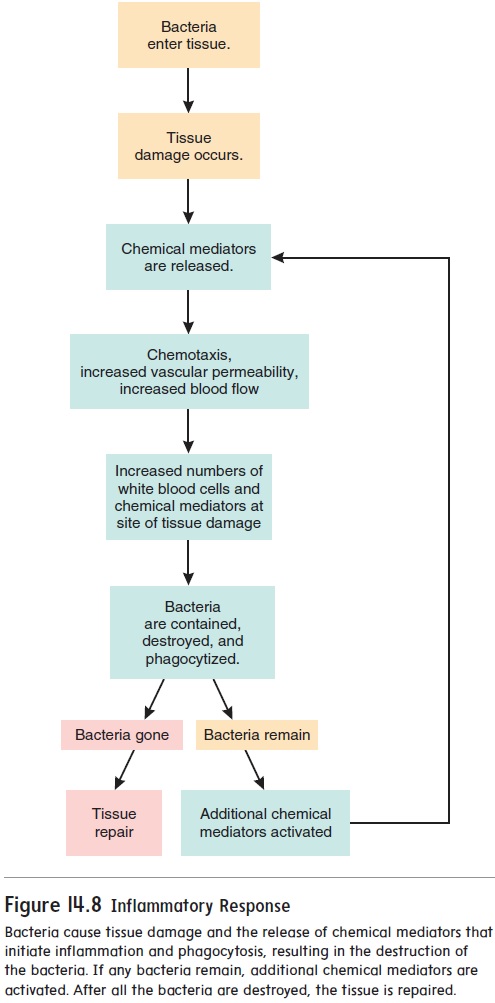
The inflammatory response to injury involves many of the chemicals and cells previously discussed. Most inflammatory responses are very similar, although some details vary, depending on the intensity of the response and the type of injury. In figure 14.8, we use a bacterial infection to illustrate an inflammatory response. Bacteria enter the tissue, causing damage that stimulates the release or activation of chemical mediators, such as histamine, prostaglandins, leukotrienes, complement, and kinins. These chemicals produce several effects: (1) Vasodilation increases blood flow and brings phagocytes and other white blood cells to the area; (2) phagocytes leave the blood and enter the tissue; and (3) increased vascular permeability allows fibrinogen and complement to enter the tissue from the blood. Fibrinogen is con-verted to fibrin , which isolates the infection by walling off the infected area. Complement further enhances the inflammatory response and attracts additional phagocytes. This process of releasing chemical mediators and attracting phago-cytes and other white blood cells continues until the bacteria are destroyed. Phagocytes remove microorganisms and dead tissue, and the damaged tissues are repaired.
Inflammation can be local or systemic. Local inflammation is an inflammatory response confined to a specific area of the body. Symptoms of local inflammation include redness, heat, and swelling due to increased blood flow and increased vascular permeability, as well as pain caused by swelling and by chemical mediators acting on pain receptors. The tissue destruction, swelling, and pain lead to loss of function .
Systemic inflammation is an inflammatory response that isgenerally distributed throughout the body. In addition to the local symptoms at the sites of inflammation, three additional features can be present:
1. Red bone marrow produces and releases large numbers of neutrophils, which promote phagocytosis.
2. Pyrogens (p′r̄o-jenz; fever-producing), chemicals releasedby microorganisms, neutrophils, and other cells, stimulate fever production. Pyrogens affect the body’s temperature-regulating mechanism in the hypothalamus in the brain. As a consequence, heat production and conservation increase, raising body temperature. Fever promotes the activities of the immune system, such as phagocytosis, and inhibits the growth of some microorganisms.
3. In severe cases of systemic inflammation, vascular permeability can increase so much that large amounts of fluid are lost from the blood into the tissues. The decreased blood volume can cause shock and death (see Clinical Impact “Circulatory Shock”).
Related Topics