Chapter: Basic & Clinical Pharmacology : Agents Used in Dyslipidemia
Inhibitors of Intestinal Sterol Absorption
INHIBITORS OF INTESTINAL STEROL
ABSORPTION
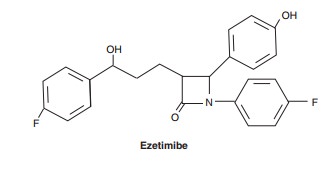
Ezetimibe is the first member of a group of drugs that inhibitintestinal
absorption of phytosterols and cholesterol. Its primary clinical effect is
reduction of LDL levels. In one trial, patients receiving ezetimibe in
combination with simvastatin had mar-ginal, but not statistically significant,
increases in carotid intimal-medial thickness (IMT) compared with those
receiving simvastatin alone. Interpretation of this observation is difficult
for several reasons, including the fact that baseline IMT was unexpectedly
small, probably due to prior lipid-lowering therapy. Because reducing LDL
levels by virtually every modality has been associ-ated with reduced risk of
coronary events, it is reasonable to assume that reduction of LDL by ezetimibe
will have a similar impact. Further studies are pending.
Chemistry & Pharmacokinetics
Ezetimibe
is readily absorbed and conjugated in the intestine to an active glucuronide,
reaching peak blood levels in 12–14 hours. It undergoes enterohepatic
circulation, and its half-life is 22 hours. Approximately 80% of the drug is
excreted in feces. Plasma con-centrations are substantially increased when it
is administered with fibrates and reduced when it is given with cholestyramine.
Other resins may also decrease its absorption. There are no sig-nificant
interactions with warfarin or digoxin
Mechanism of Action
Ezetimibe is a
selective inhibitor of intestinal absorption of choles-terol and phytosterols.
A transport protein, NPC1L1, appears to be the target of the drug. It is
effective even in the absence of dietary cholesterol because it inhibits
reabsorption of cholesterol excreted in the bile.
Therapeutic Uses & Dosage
The
effect of ezetimibe on cholesterol absorption is constant over the dosage range
of 5–20 mg/d. Therefore, a single daily dose of 10 mg is used. Average
reduction in LDL cholesterol with ezetimibe alone in patients with primary
hypercholesterolemia is about 18%, with minimal increases in HDL cholesterol.
It is also effective in patients with phytosterolemia. Ezetimibe is synergistic
with reductase inhibitors, producing decrements as great as 25% in LDL
choles-terol beyond that achieved with the reductase inhibitor alone.
Toxicity
Ezetimibe does not
appear to be a substrate for cytochrome P450 enzymes. Experience to date
reveals a low incidence of reversible impaired hepatic function with a small
increase in incidence when given with a reductase inhibitor. Myositis has been
reported rarely.
Related Topics