Chapter: Pathology: Central Nervous System Pathology
Infections - Central Nervous System
INFECTIONS
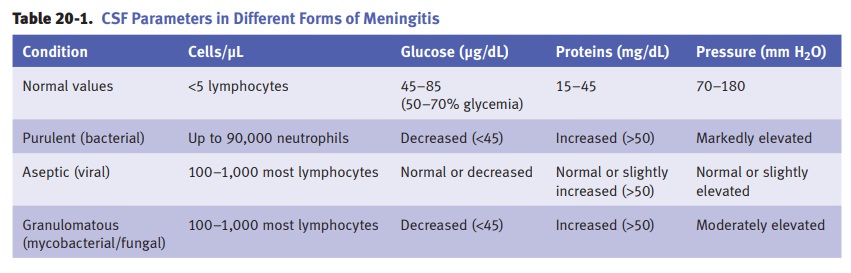
Meningitis is inflammation of the 2 inner meningeal
layers, the pia and the arach-noid.
Acute aseptic (viral) meningitis is caused by leptomeningeal
inflammation due to viruses (enterovirus most
frequent); the inflammation produces a lymphocytic infiltration of
leptomeninges and superficial cortex. Patients present with fever, signs of
meningeal irritation, and depressed consciousness. Mortality is low. Viral
meningitis carries a better prognosis than bacterial meningitis.
Acute viral meningitis is the
most common neurologic symptom associated with primary HIV infection; it
presents around the time of seroconversion with an acute confusional state.
Symptoms resolve after 1 month with supportive care.
Acute purulent (bacterial) meningitis is a purulent leptomeningeal
inflammation.
•
Streptococcus pneumoniae is the most common cause of meningitis in
infants, young children, and adults.
•
Neonates are infected most frequently with group B streptococci but
Eschericia coli causes a greater number of fatalities.
•
Neisseria meningitidis is seen in teens and young adults and is
often associated with a maculopapular rash.
•
The incidence of Listeria monocytogenes increases after age 50.
This pathogen also tends to infect people with poor cell-mediated immunity.
The leptomeninges are opaque
on gross examination. Microscopic examination shows neutrophilic infiltration
of the leptomeninges, extending variably to cortex.
Diffuse cerebral edema
carries a risk of fatal herniations. The classic triad of bacte-rial meningitis
is fever, nuchal rigidity, and altered mental status.
Mycobacterial meningoencephalitis can be caused by Mycobacterium tuberculo-sis or atypical mycobacteria. It occurs in patients
who have reactivation of latent infection
and immunocompromised patients such as AIDS patients (Mycobacterium avium-intracellulare).
Diagnosis requires microscopy/culture of large volumes of CSF. MRI is the imaging test of choice and shows basal meningeal
enhancement and hydrocephalus. It usually involves the basal surface of the
brain, and may cause characteristic tuberculomas within the brain and dura
mater.
The viral encephalitides have common features of
perivascular cuffs, microglial nodules, neuron loss, and neuronophagia.
Clinical manifestations are variable, and can include mental status change, fever,
and headache, often progressing to coma.
•
Arthropod-borne forms can be due to St. Louis, Eastern and Western
equine, and Venezuelan encephalitides.
•
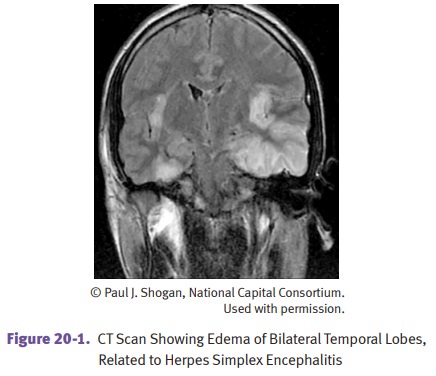
Herpes simplex type 1 produces a characteristic hemorrhagic necrosis of tem-poral lobes.
Cowdry type A bodies are intranuclear inclusions seen in neurons and glial cells.
•
Rabies has characteristic Negri
bodies in the cytoplasm of hippocampal and
Purkinje cells.
•
HIV encephalopathy shows histopathology of
microglial nodules and diag-nostic multinucleated giant cells. Spinal
involvement leads to vacuolar myelop-athy, which is similar to vitamin B12
deficiency–associated subacute combined degeneration.
•
Progressive multifocal
leukoencephalopathy (PML) is caused by JC poly-omavirus. It occurs in immunocompromised
patients and patients taking immunomodulatory therapies. Neurologic symptoms
are varied and include impairment of cognition and motor function. There is no
specific antiviral drug and mortality is high. Tissue sections show areas of
demyelination and enlarged oligodendrocytes.
Fungal meningoencephalitides. Candida, Aspergillus, Cryptococcus, and Mucor spe-cies are the most
frequent agents. Aspergillus and Mucor have a marked tropism for blood
vessels, which leads to vasculitis, rupture of blood vessels, and hemorrhage. Cryptococcus causes diffuse
meningoencephalitis, which leads to invasion of the brain through the Virchow-Robin space (a continuation of the
subarachnoid space around blood vessels entering the neuropil) and soap bubble
lesions.
Toxoplasmosis is caused by the protozoan
parasite Toxoplasma gondii. It is common in AIDS patients, and the
condition causes cerebral abscess with central necrosis and chronic
inflammation. MRI/CT scan shows a characteristic ring-enhancing lesion.
Cerebral abscess can occur as a result of
either hematogenous dissemination or direct spread from contiguous
foci. Systemic predisposing conditions
include acute bacterial endocarditis, cyanotic heart disease (right-to-left
shunt), and chronic pul-monary abscesses. Local
predisposing conditions include mastoiditis, paranasal sinusitis, acute
otitis, open fracture, and previous neurosurgery. CT/MRI scan
char-acteristically shows a ring-enhancing lesion. Clinical manifestations
include signs of increased intracranial pressure (headache, vomiting, and
papilledema). Focal neurological deficits vary depending on the site of lesion.
Subacute sclerosing panencephalitis is a rare complication of
measles (rubeola) virus infection. Persistent immune-resistant
measles virus infection causes slow-virus encephalitis. The typical scenario is
a child who had measles age <2 and then 6–15 years later develops progressive
mental deterioration with seizures. Subacute sclerosing panencephalitis may be
fatal in 1–2 years once it develops.
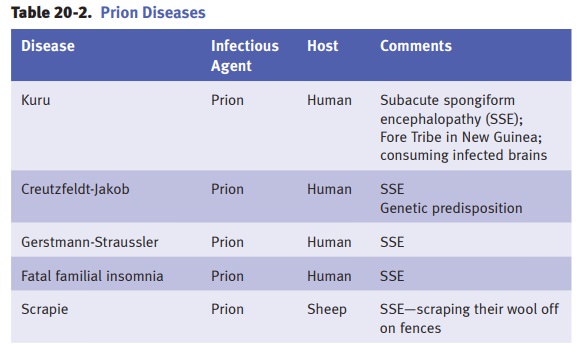
Creutzfeldt-Jakob disease (CJD) is the most common
human transmissible spon-giform encephalopathy due to a prion (a protein with
the capacity to be an infec-tious agent) that can change the conformation of
normal prion protein(s). This can lead to rapidly progressive dementia, memory
loss, personality changes, and hallucinations.
•
The prion protein (PrP)
is a 30-kD protein normally present in neurons. It is encoded by a single-exon
gene on chromosome 20. Its normal conformation is an α-helix: PrPc. In disease states, PrPc changes to a β-pleated sheet con-formation: PrPsc. A low rate of spontaneous change results in sporadic cases of
CJD. Mutations of PrP result in hereditary cases of CJD. PrPsc facilitates conformational
change of other PrPc molecules into PrPsc.
•
PrPsc
is responsible for cerebral pathologic
changes, characteristically resulting in spongiform change. This change is
a fine vacuolization of the neuropil in the gray matter (especially cortex),
which is due to large membrane-bound vacuoles within neuronal processes. There
is an associated neuronal loss and astrogliosis. Kuru plaques are deposits of
amyloid composed of altered PrP protein.
•
About 85% of Creutzfeld-Jakob cases are sporadic, and 15% are
familial. Affected patients are typically middle-aged to elderly patients who
develop rapidly progressive dementia and memory loss with startle myoclonus or
other involuntary movements. Typical EEG changes may be diagnostic. Death
occurs within 6–12 months.
•
Variant Creutzfeldt-Jacob disease occurs in younger patients and
results from exposure to bovine spongiform encephalopathy.
HIV-associated neurocognitive disorder (HAND) presents as cognitive decline
with behavioral changes and motor symptoms.
Diagnosis is based on clinical features and the exclusion of other etiologies.
Related Topics