Chapter: Basic Radiology : Imaging of Joints
Imaging of Joints: Techniques and Normal Anatomy
Imaging of Joints
TECHNIQUES AND NORMAL ANATOMY
Radiography
Conventional radiography is the
most commonly used im-aging technique to evaluate the joints of the
musculoskeletal system. This technique should always be the first imaging study
performed in a patient suspected of having joint prob-lems. Radiography has the
following important advantages: It is almost universally available, is
relatively inexpensive compared to other imaging studies and delivers only a
small radiation dose to the patient. When possible, orthogonal projections
should be obtained, meaning two images of the joint that are perpendicular to
each other (usually a frontal projection in either in the anteroposterior [AP]
or pos-teroanterior [PA] directions and a lateral). In some instances oblique
images may also be obtained, depending on the preferences of the referring
physician or radiologist or the clinical situation. In certain instances it may
also be impor-tant to obtain images of the joint proximal and distal to the
injury. Examples of this include the forearm and lower leg (paired bones), as
the joints proximal and distal are often in-jured. Because conventional
radiography uses ionizing radi-ation, it should be used judiciously, especially
in pediatric patients and pregnant women.
Historically, radiographic images
were printed on film. However, with widespread adoption of PACS (picture
archiv-ing and communications system), images can be electroni-cally processed
and viewed on computer work screens. These images then can be transmitted
anywhere electronically via the Internet.
Conventional Tomography
Conventional tomography is
mentioned mainly for historical interest. High radiation dose, relatively poor
image resolution, and imaging that is only possible in one plane were its major
disadvantages. The technique has been almost totally re-placed by other imaging
tests, especially computed tomo-graphic (CT) and magnetic resonance (MR)
imaging. Orthopantograms are one of the few remaining vestiges of this imaging
technique.
Arthrography
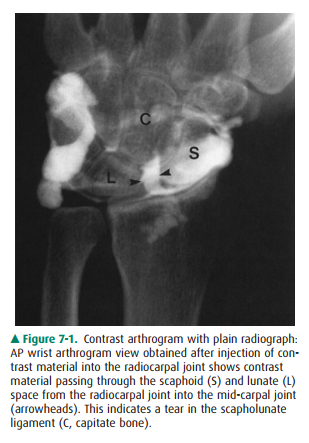
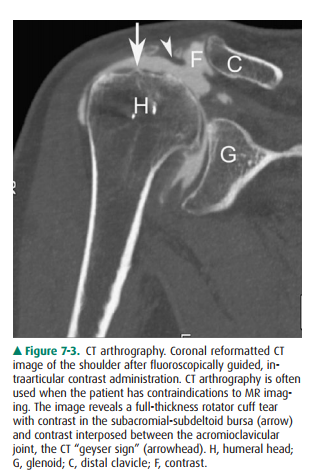
Arthrography is a technique in
which contrast is injected into the joint using fluoroscopic guidance. The
joint is then im-aged using radiography, CT, or MR imaging or a combina-tion of
these techniques. The injected contrast may be an iodine-containing
water-soluble compound (eg, Conray), subsequently imaged with radiography or CT
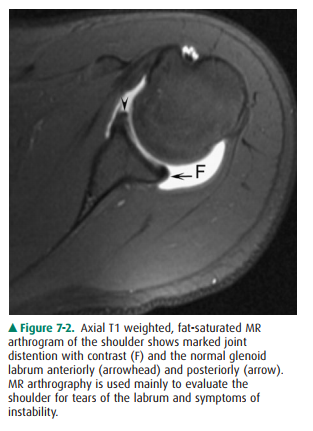
(Figure 7-1). Alternatively, a paramagnetic compound (eg, gadolinium
pentazocine) may be injected and imaged with MRI. MR arthrographic images of
the joint may also be performed after intravenous injection of the paramagnetic
contrast agent, although this technique does not distend the joint, and thereby
is not used commonly today. MR arthrography is mainly used to evaluate the
labrum of the hip or glenohumeral joint (Figure 7-2) but is also useful in the
evaluation of the structures of the wrist and elbow joints. CT arthrography,
and less commonly conventional arthrography can be useful in patients who
cannot undergo, or have contraindications to, MR imaging (Figure 7-3).
Computed Tomography
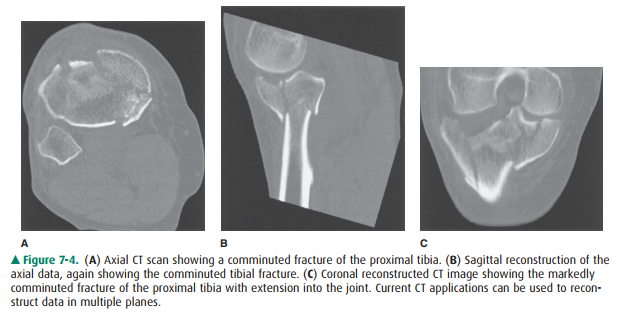
Computed tomography (CT), a
technique that makes indi-vidual axial (transverse) slices of the patient, uses
the same ionizing radiation as in conventional radiography. CT technique has
been vastly improved in the past decade. The development of spiral or helical
CT has major advantages over earlier CT technology. With the spiral CT
technique, axial (transverse) images are acquired much more rapidly with
dramatic decreases in radiation dose. For instance, a CT of the chest, abdomen,
and pelvis can be performed in about 16 seconds. CT data is stored in
three-dimensional packets that can then be reconstructed and displayed in
al-most any other plane. The most common images recon-structed from the axial
plane are the sagittal and coronal planes (Figure 7-4).
Magnetic Resonance Imaging
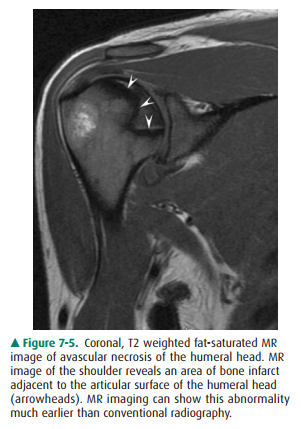
MR imaging has revolutionized the
imaging evaluation of almost all body areas, but particularly those of the
central nervous system and musculoskeletal system. It has tremen-dous
advantages over other imaging modalities in the eval-uation of joints because
of its excellent soft-tissue contrast, high resolution, and ability to image in
every plane. This technique may show pathophysiologic events even before they
are seen on conventional radiographs or CT, for exam-ple, revealing the early
changes of avascular necrosis (Figure 7-5). Because of its exquisite
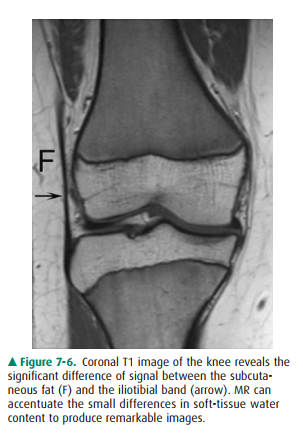
soft-tissue contrast, MR imag-ing allows radiologists to visualize subtle
differences in soft tissues that had never before been seen with other imaging
modalities. For example, the subtle contrast between fat and muscle seen on a
conventional radiographs or CT is dra-matically highlighted with the use of MR
imaging because of their very different chemical compositions (Figure 7-6). MR
imaging can also depict subtle changes within the bone marrow cavity, an area
difficult to evaluate with conven-tional radiography or CT. Therefore, MR
imaging is a tremendous aid to preoperative evaluation of any patient who has
unexplained joint pain or who has had joint trauma. One of the major
disadvantages of MR imaging is that some patients with claustrophobia cannot tolerate
the prolonged imaging time in the small bore of the magnet. In addition,
patients with metallic foreign bodies or non-MR-compatible medical devices or
hardware have contraindi-cations to MR imaging. Concerns include motion of the
objects, abnormal electrical arcs resulting in burns, and de-vice malfunction.
Ultrasonography
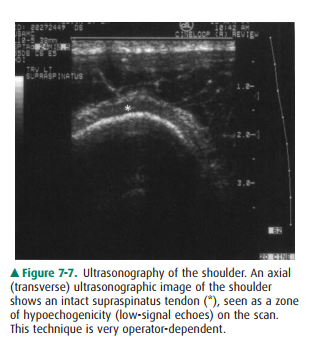
Ultrasonography, first developed
for use in World War II for detection of submarines, was adopted after the war
for use in medical imaging. High-frequency transmission of sound can be used to
evaluate the soft tissues, tendons, ligaments, and even the cartilage of the
joint. The ultrasound waves cannot be transmitted through cortical bone, so the
intramedullary cavity cannot be imaged with this technique. Ultrasound is used
more extensively in Europe than in the United States; however, there is
increasing interest in this modality within the United States. The main
drawback of this modality is that it is highly user-dependent, relying heavily
on the skill of the operator (Figure 7-7).
Radionuclide Imaging (Nuclear Medicine Bone Scans)
Radionuclide imaging uses
radioactive materials that are injected intravenously and then localize in
regions of ab-normally increased blood flow (hyperemia), increased
os-teoblastic activity, or heightened metabolic activity. The major uses of
bone scanning are in patients suspected of having metastatic disease or
infection. This modality is very sensitive, but it has limited specificity, and
often the findings must be correlated with other imaging modalities, especially
radiography. Therefore, this technique is not usually used as a primary
modality for the evaluation of joint disease.
Anatomy of the Normal Joint
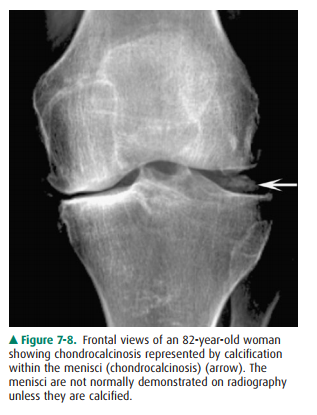
The typical normal synovial joint
consists of at least two ar-ticulating bones enclosed in a synovium-lined joint
capsule. The apposing bony surfaces are covered by smooth articular cartilage
(hyaline cartilage). On radiographs, the normal joint has a separation between
the adjacent bones represent-ing the region occupied by the hyaline or
articular cartilage, menisci, and joint fluid (the so-called articular space)
de-pending on which joint is imaged. Because of the limited soft-tissue
contrast of the technique, these structures are not normally depicted on
radiographs unless they are calcified (Figure 7-8). However, MR imaging
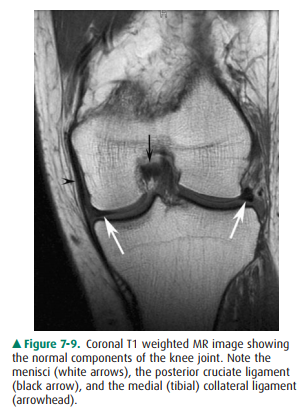
exquisitely shows the components of the normal joint (Figure 7-9).
Joint Disease
The clinical signs and symptoms
of joint disease are mani-festations of abnormal function such as reduced
mobility, hypermobility, and pain. Altered function may be due to pain,
discomfort, apprehension, or instability. The wide range of joint abnormalities
is summarized below, and many of these processes are discussed in the
exercises. Any of these signs may occur in isolation or in combination with any
others.
Radiographically, joint disease
may be diagnosed by any of the following:
·
Incongruity of the articulating bone as is seen with
dislo-cations, for example, traumatic dislocation or disloca-tions caused by
arthropathies such as lupus arthritis or rheumatoid arthritis.
·
Irregularity of articulating bone surfaces and margins, as in
erosions (eg, in psoriasis or gout).
·
Increased density or sclerosis of articulating bone surface
(also called “eburnation”), as in osteoarthritis.
·
Bony outgrowths (proliferation) at bone ends, known as
osteophytes.
· Diffuse decrease of bone density
adjacent to articular surfaces, described as juxtaarticular or periarticular
os-teopenia (eg, rheumatoid arthritis, tuberculous arthritis).
·
Focal, well-defined, spherical lucencies within subchon-dral
bone, known as subchondral cysts or geodes (eg, os-teoarthritis, rheumatoid
arthritis).
·
Loss of articular joint space from articular cartilage
de-struction (eg, septic arthritis, osteoarthritis).
·
Accumulation of excess joint fluid within the joint (joint
effusion). Excess joint fluid is a common manifestation of joint disorders. The
fluid may be synovial fluid, blood, or even pus, depending on the etiology of
the joint disease.
·
Calcification of articular (hyaline) cartilage or
fibrocarti-lage (chondrocalcinosis), or intraarticular soft-tissue cal-cification
such as that seen in scleroderma or polymyositis or dermatomyositis.
·
Synovial proliferation or abnormal increase in the syn-ovial
lining, such as that seen with pigmented villonodu-lar synovitis (PVNS).
Related Topics