Chapter: Basic Radiology : Imaging of Joints
Exercise: Miscellaneous Joint Disorders
EXERCISE 7-5.
MISCELLANEOUS JOINT DISORDERS
7-18. The most likely
diagnosis for Case 7-18 (Figure 7-46) is
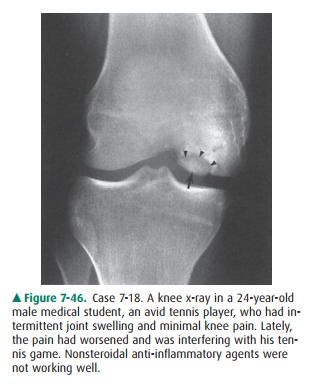
A.
synovial osteochondromatosis.
B.
pigmented villonodular synovitis.
C.
avascular necrosis of the femoral condyle.
D.
osteochondritis dissecans (OCD) of the femoral condyle.
7-19. The most likely
diagnosis for Case 7-19 (Figure 7-47) is
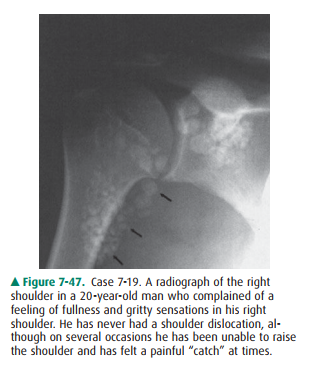
A.
hemochromatosis.
B.
synovial osteochondromatosis.
C.
pigmented villonodular synovitis.
D.
calcified Heberden’s nodes.
7-20. The most likely
diagnosis for Case 7-20 (Figure7-48) is
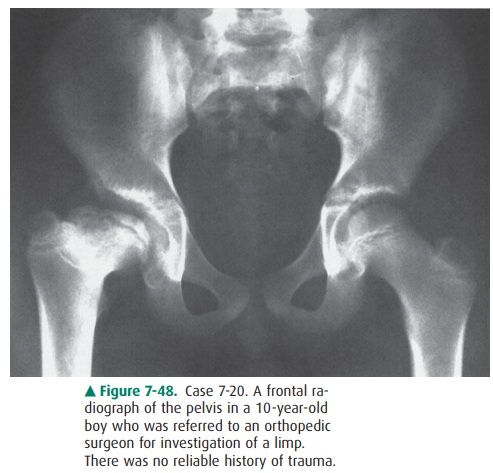
A. chronic changes of transient synovitis of the right hip.
B. chronic changes of slipped capital femoral epiph-ysis
(epiphysiolysis).
C.
chronic changes of Legg-Calvé-Perthes disease of the right hip.
D.
neurofibromatosis.
7-21. Concerning Case
7-21 (Figure 7-49), the observa-tions include all of the following except
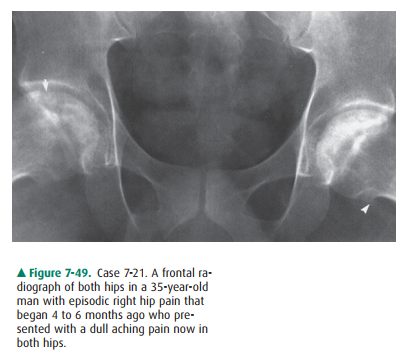
A.
osteophyte in both femoral heads.
B.
irregularity and loss of spherocity of the right femoral head.
C.
depression/subchondral fracture of right femoral head.
D.
bilateral acetabular sclerosis.
Radiologic Findings
7-18. The AP view of the right knee
(Figure 7-46) shows an ovoid bony fragment on the inner aspect of the me-dial
femoral condyle (arrow) separated from the femur by a lucency (arrowheads).
This appearance is diagnostic of osteochondritis dissecans (OCD) of the knee (D
is the correct answer to Question 7-18).
7-19. The radiograph of
the right shoulder in Figure 7-47 shows multiple rounded calcific bodies
overlying the proximal humerus and glenoid process of the scapula. The
distribution of these is within the joint and axillary recess (arrows). This
appearance is classic for synovial osteochondromatosis (SOC) (B is the correct
answer to Question 7-19).
7-20. The radiograph of
the pelvis in Figure 7-48 shows collapse of the right capital femoral
epiphysis, which is broad and short and forms an acute angle with the shaft of
the femur. The femoral head is displaced lat-erally and is not completely
covered by the mildly re-modeled acetabulum. The left hip is normal. The
findings are characteristic of the late changes in Legg-Calvé-Perthes disease
(C is the correct answer to Question 7-20).
7-21. The radiograph of
both hips in Figure 7-49 demon-strates that the right femoral head is no longer
smooth and spherical (loss of spherocity), and this is due to the presence of
subchondral collapse in the superiolateral aspect (arrow). The left femoral
head is still spherical but shows sclerosis. Also note the marginal
osteo-phytes arising from the inferior and medial aspect of the left femoral
head (arrowhead). The acetabuli are normal, and these radiographic features are
typical of avascular necrosis (osteonecrosis) of the femoral head (D is the
correct answer to Question 7-21).
Discussion
Osteochondritis dissecans is a
bone disorder that produces joint symptoms because of the intraarticular
location of the abnormality. OCD, as classically demonstrated in Figure 7-46,
is seen on the radiograph as a semicircular focus of bone and overlying
cartilage separated from the convex articular sur-face of the native bone by a
lucency. The etiology is uncertain, but current opinion favors repetitive
microtrauma and vascu-lar insult to the subchondral bone. Almost any joint may
be af-fected, but the knee (distal femur), ankle (dome of the talus), and elbow
(capitellum) joints are the most commonly involved sites. The disease is
slightly more common in active young men but is increasingly being encountered
in young women because they are more actively involved in athletics today. In
the knee, OCD most commonly involves the non-weight-bearing aspect of the
medial femoral condyle (ie, the inner aspect and area shown in Figure 7-46) and
the lateral femoral condyle. MR im-aging is the most appropriate modality to
stage the lesion, as-sess the stability of the fragment, and plan definitive
treatment. CT or CT arthrography is an alternate modality to use in pa-tients
who cannot undergo MR imaging.
Synovial osteochondromatosis is a
joint abnormality char-acterized by the presence of cartilaginous and osseous
loose bodies within the synovial cavity in the joint. The exact cause is not
known, but “primary” SOC is thought to be caused by synovial metaplasia.
“Secondary” OCD is assumed to be due to fractures of osteophytes or articular
cartilage that shed into the joint cavity. If calcified, these intraarticular
fragments can be visualized on conventional radiographs (Figure 7-47, ar-rows).
MR imaging is the best modality to use to show both ossified and nonossified
intraarticular fragments and to eval-uate the other soft-tissue structures
around the joint.
Pigmented villonodular synovitis
(PVNS) is a condition of unknown etiology characterized by hyperplasia or
excessive villous proliferation of the synovium. This condition may occur in a
single joint (localized form) or involve multiple joints (diffuse form).
Thought to be caused by hemorrhage, PVNS shows hemosiderin-laden macrophages
within the syn-ovium best appreciated by gross examination. Radiographs often
show a joint effusion with preservation of the articular space and normal bone
mineral density. The later stages of the disease result in erosions on both
sides of the joint. Joint aspiration yields dark brown fluid (“chocolate”
effusion) due to the presence of the hemosiderin-laden macrophages. MR imaging
is an excellent preoperative test to evaluate PVNS because the pigmented
material (hemosiderin) shows low signal intensity on both the short TE
(T1-weighted) and the long TE (T2-weighted) MR sequences. The gradient echo
se-quence is particularly sensitive for the detection of hemo-siderin. In fact,
this finding is a very specific appearance for this disease.
Heberden’s node is a
disfigurement of the interphalangeal joints as a result of severe
osteoarthritis. Initially, it is due to soft-tissue inflammatory changes and is
subsequently due to bony changes at the distal interphalangeal joints. It is
more commonly seen in female patients.
Osteonecrosis can occur in any
bone and is associated with a variety of disorders, including sickle cell
hemoglo-binopathy, Gaucher’s disease, SLE, pancreatitis, alcoholism, steroid
treatment, and barotrauma. When the process occurs at an articular surface, it
is known as avascular necrosis or os-teonecrosis; when it occurs in the
metaphysis of the bone, it is commonly referred to as a bone infarct. Eponyms
have been used to designate osteonecrosis in certain sites. For example,
Perthes’ disease (Legg-Calvé-Perthes disease) is the eponym used to refer to
idiopathic osteonecrosis of the femoral head occurring in a child as shown in
Case 7-20 (Figure 7-48).
Other common eponyms include
Freiberg’s infarction, (avas-cular necrosis of the head of the second or third
metatarsal), Kohler’s disease (tarsal navicular), Panner’s disease (capitel-lum
of the humerus), and Kienbock’s disease (carpal lunate). The exact mechanism of
the development of osteonecrosis is unknown, although bone-marrow edema after
thrombosis and occlusion of the osseous capillaries and end arterioles are
believed to be primarily responsible.
Conventional radiographs are much
less sensitive compared to MR regarding the detection of early osteonecrosis.
Increased areas of serpiginous sclerosis and osteolysis can be noted on
conventional radiographs; however, these abnormalities found relatively late
compared to MR imaging, and therefore treat-ment outcome of the disease may be
delayed or adversely af-fected (Figure 7-49). Importantly, if the disease is
not diagnosed and treated early, the affected bone may go through a phase of
subchondral collapse and become deformed. Subsequently, complications of
secondary osteoarthrosis will develop in the affected joint. Traditionally,
nuclear medicine bone scanning has been used in this setting, but today MR
imaging is the most sensitive available modality for the early diagnosis of
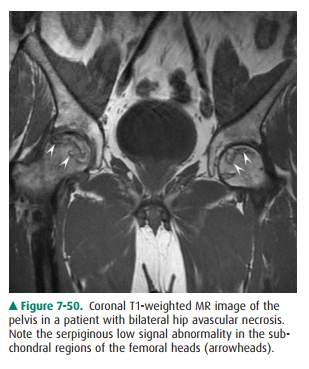
this dis-ease (Figure 7-50).
Hemochromatosis is a rare
disorder of iron metabolism, in which iron is deposited in the skin,
parenchymal organs, and articular cartilage. This predisposes the joint to
degenerative disease. Arthritis due to hemochromatosis is characterized by loss
of joint space and formation of peculiar hooked osteo-phytes, especially at
metacarpal heads.
Related Topics