Chapter: Medical Microbiology: An Introduction to Infectious Diseases: Cryptococcus, Histoplasma, Coccidioides, and Other Systemic Fungal Pathogens
Histoplasmosis: Clinical Aspects
HISTOPLASMOSIS :CLINICAL ASPECTS
MANIFESTATIONS
Most cases of H. capsulatum infection are asymptomatic or show only fever and cough for a few days or weeks. Mediastinal lymphadenopathy and slight pulmonary infiltrates may be seen on x-rays. The histoplasmin skin test becomes positive after about 3 weeks. More severe cases may have chills, malaise, chest pain, and more extensive infiltrates, which usually resolve nonetheless. A residual nodule may continue to enlarge over a period of years, causing a differential diagnostic problem with pulmonary neoplasms. Progressive pulmonary disease occurs in a form similar to that of pulmonary tuberculosis, including the development of cavities, with sputum production, night sweats, and weight loss. The course is chronic and relapsing, lasting many months to years.
Disseminated histoplasmosis generally appears as a febrile illness with enlargement of reticuloendothelial organs. The CNS, skin, gastrointestinal tract, and adrenal glands may also be involved. Painless ulcers on mucous membranes are a common finding. The course is typically chronic, with manifestations that depend on the organs involved. For example, chronic bilateral adrenal failure (Addison’s disease) may develop when the adrenal glands are involved.
DIAGNOSIS
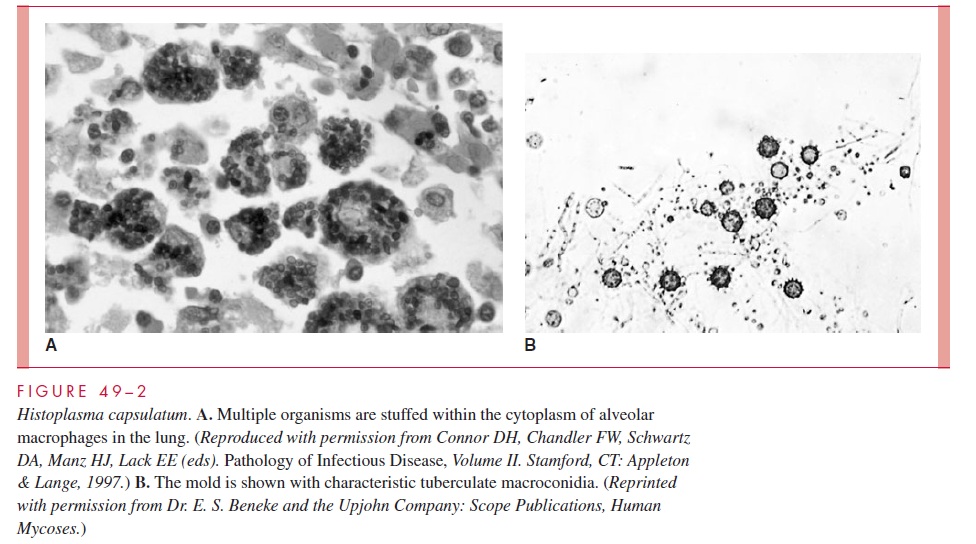
In most forms of pulmonary histoplasmosis, the diagnostic yield of direct examinations or culture of sputum is low. In disseminated disease, blood culture or biopsy samples of a reticuloendothelial organ are the most likely to contain Histoplasma. Bone marrow culture has the highest yield. Because of their small size, the yeast cells are difficult to see in potassium hydroxide (KOH) preparations, and their morphology is not sufficiently distinc-tive to be diagnostic. Selective fungal stains such as methenamine silver demonstrate the organism but may not differentiate it from other yeasts. Hematoxylin and eosin (H&E)–stained tissue or Wright-stained bone marrow often demonstrates the organisms in their intracellular location in macrophages (see Fig 49–2). Specimens must be examined carefully under high magnification. Identification of culture isolates requires demonstra-tion of the typical conidia and dimorphism. Demonstration of specific mycelial antigens by immunodiffusion (exoantigen test) may be used in place of dimorphism demonstration. Nucleic acid probes have been developed for culture identification.
Antibodies can be detected during and following infection, but their usefulness in the endemic area is limited by false-negative results and cross-reactions in patients with blastomycosis. Rising antibody titers are suggestive of dissemination or relapse. The histoplasmin skin test is useful for epidemiologic studies but is not used for diagnosis or management of individual cases. Cultural isolation or clear histologic demonstration is necessary for a firm diagnosis. A circulating polysaccharide antigen has been demon-strated in serum and urine by enzyme immunoassay (EIA) in more than 90% of patients with disseminated disease.
TREATMENT
Primary infections and localized lung lesions usually resolve without treatment. Ampho-tericin B remains the treatment of choice, but its toxicity limits its use to cases of extensive disease such as progressive pulmonary and disseminated histoplasmosis. Itraconazole and ketoconazole have been effective for treatment and for suppression in AIDS patients with
Related Topics