Chapter: XML and Web Services : Applied XML : Applied XML in Vertical Industry
Health Care: Health Level Seven (HL7)
Health Care
Besides insurance, health care is the most heavily document-dominated
industry. Every aspect of the care of patients must be documented, from patient
acquisition and appointments, to specific treatment and payment. Therefore,
many groups have emerged to solve the various documentation challenges
associated with health care. In this section, we feature a few of those health
care–related industry standards.
Much of the recent activity in XML-enabling health care can be
attributed to one motiva-tor: The Health Insurance Portability &
Accountability Act (HIPAA) of 1996. This one law, also known as the
Kennedy-Kassebaum Act, seeks to make major changes to the way medical
information is stored and exchanged. It mandates that health care efficiency
must be improved by standardizing electronic data interchange, and information
must be maintained with the strictest confidentiality and security through the
setting and enforce-ment of standards. In particular, HIPAA calls for the
standardization of electronic patient health, administrative, and financial
data, the establishment of unique health identifiers for individuals,
employers, health plans, and health care providers, and the setting of security
standards to protect the confidentiality and integrity of “individually
identifiable health information,” past, present, or future. And this all needs
to be implemented by October 16, 2002 for the first part, and April 14, 2003
for the second. Otherwise, penal-ties up to $250,000 will apply!
XML is perfectly suited to providing all the requirements of HIPAA in a
manner that also simplifies the requirements for integration with the tons of
legacy systems that medical establishments have in place. Sounds like XML to
the rescue. Of course, there are also lots of reasons besides HIPAA why XML
should be implemented in the health care space, including platform neutrality,
prevalence of tools, greatly reduced cost, a large set of skilled XML labor,
and positive buzz—but none of these exerts as much pressure as HIPAA.
A few major standards hope to solve this problem, which is generally
known as Electronic Patient Records (EPR). The front leader in this category is
the Health Level Seven (HL7) standard. HL7 originally was a non-XML standard
but is rapidly becoming a major influence in the XML space with its next
standards release. HL7 specifies a health care industry–specific format that
covers the needs for EPR, prescriptions, and medical insurance filings as well
as medical imaging needs. Its next major release, v3.0, plans to support XML
natively and has considerable backing.
For those who are interested in medical record XML standards but can’t
wait for the HL7 release, there are a number of other efforts by organizations
aiming to “fill the gap” in meeting HIPAA requirements. These include the
CISTERN specification, which builds upon HL7’s prior releases. DocScope and
Xchart are other private efforts to tackle the EPR problem.
In general, a growing body of work is being pursued in creating XML
formats specifi-cally for the health care industry, and especially the medical
records industry. For more information, check out the “Healthcare” listing in
the “XML in Industry” section of the www.xml.org
Web site.
Health Level Seven (HL7)
Health Level Seven, whose name refers to the top level (the application
level) of the International Standards Organization’s (ISO) communications model
for Open Systems Interconnection (OSI), is an American National Standards
Institute (ANSI) approved Standards Developing Organization (SDO) focused on
the health care arena. SDOs pro-duce standards for a wide variety of domain
areas in the health care space, ranging from pharmaceutical, medical devices,
imaging, and insurance. The HL7 SDO focuses on standards for clinical and
administrative data. More specifically, HL7 produces standards for the
exchange, management, and integration of data that supports clinical patient
care and the management, delivery, and evaluation of health care services. The
goal of the Ann Arbor, Michigan–based nonprofit organization is to service its
members, which include providers, vendors, payers, consultants, government
groups, and others who have an interest in the development and advancement of
clinical and administrative standards for health care. HL7 is also international
in scope, with applications in Australia, Canada, China, Finland, Germany,
India, Japan, Korea, The Netherlands, New Zealand, Southern Africa,
Switzerland, and the United Kingdom.
The application level of the OSI model isn’t concerned with the lower-level
aspects of data communication (such as transport and routing) but rather
addresses application data definition, exchange, error checking, security
checks, participant identification, availabil-ity checks, and data structure.
Created in 1989, HL7 has been standardizing clinical and administrative
data for health care, utilizing an EDI-like messaging specification. However,
its latest release is a full-scale movement to XML. The most widely adopted of
its specifications is patient and financial administration, which solves
specific transactional issues such as admitting new patients to a hospital. HL7
solves the major problem of sharing this patient data with all the systems in a
hospital that need to know about new patients. This standardization, widely
used for patient administration, certain kinds of laboratory data, and to some
extent for clinical observations, results in a high level of penetration by HL7
in the industry. Over 90 percent of U.S. hospitals use some portion of the HL7
standard, which is the highest adoption of any specification in health care.
However, the scope and focus of the specification still leaves a lot of room
for standardization. The specification was started so many years ago and was
built up by accretion. The result was so broad based that it became difficult
to add new functionality in the 1990s. As a result, the HL7 man-aging
organization realized that it needed to go back and rethink the whole approach.
It needed a more coherent model, and XML was the answer.
The HL7 created the Reference Implementation Model (RIM), which resulted
in a grand simplification of the messages based on XML. The group working on
the specification was looking at the fact that despite the best efforts of HL7,
and despite intensive work to computerize patient records, the effort to move
from paper-based to computer-based sys-tems had stalled. About 85 percent of
clinical information was still paper based.
Therefore, even if hospitals used document management systems, the
results were printed, and most still used paper, rather than the electronic
form. The group realized that the attempt to computerize info relied on a
highly regularized, normalized data model that did not fit clinical practice
and the way doctors think of the clinical encounter. The various doctors
looking at XML saw a means to create a new approach to standardizing clinical
information that took advantage of the sparsely populated tree structure of
XML. The result was a models-based approach using the RIM, a product of seven
years of work in the industry. The final product was HL7 v3.0, a new version by
number, but a completely new product in reality.
Because some countries have mandated the use of HL7 by law, there was
good reason to maintain the old HL7 interfaces. Therefore, the organization
took a scaled approach for gently moving the space from the EDI-like syntax of
v2.4 to the XML-based v3.0. This resulted in three major products and versions
of the HL7 specification:
An informative specification
called “v2.XML” that created an XML expression for the current generation of
HL7 specs.
The clinical document
architecture (CDA), approved in November 2000, which took the new approach to
standardizing clinical information using the ability of XML but didn’t produce
a formal version of the HL7 standard.
The formal HL7 v3.0, which is a
complete set of clinical messages that overlap the functionality of v2.0 but is
derived from the RIM information model.
While contributing to v3.0, the CDA is not formally part of any
specification. Instead, it helps users make the mental transition to the new
way of doing things. The CDA is based on the RIM and uses HL7 methodology for
deriving XML from a UML object model. The core component of information is what
a physician is willing to sign. The model combines the concept of a persistent
information unit, the concept of wholeness, and a signature to create an
integrity-based system. As a result, the final specification is very
elementary, almost like XHTML in its model, with a few other features related
to the information model of clinical content. Listing 22.5 shows the CDA
document hierarchy.
LISTING 22.5 CDA Document Hierarchy
(from the HL7 Web Site)
CDA Level One
CDA
Level Two
Level
Two :: Progress
Note
Level
Two :: Cardiology
Progress Note
Level
Two :: Endocrinology
Progress Note
Level
Two :: Diabetes
Mellitus Progress Note
CDA
Level Three
Level
Three :: Progress
Note
Level
Three :: Cardiology
Progress Note
Level
Three :: Endocrinology
Progress Note
Level
Three :: Diabetes
Mellitus Progress Note
HL7 version 3.0 encapsulates all the functionality of previous versions
but uses the new reference model and architecture for its representation. It
also allows multiple representa-tions of the expression, not limiting itself to
XML. For example, one can express HL7 3.0 in IDL and ASN as well. The current
functionality of HL7 is covered in Table 22.2.
TABLE 22.2 HL7 Functionality
Functionality : Definition
Control : Message definitions and interchange protocols
Patient administration : Admit, discharge, transfer, and demographics
Order entry : Orders for clinical services and observations, pharmacy,
dietary, and supplies
Query : Rules applying to queries and to their responses
Financial management : Patient accounting and charges
Observation reporting : Observation report messages
Master files : Health care application master files
Medical records/ : Document management
information management : services and resources
Scheduling : Appointment scheduling and resources
Patient referral : Primary care referral messages
Patient care : Problem-oriented records
Laboratory automation : Equipment status, specimen status, equipment inventory,
equipment comment, equipment response, equipment noti- : fication, equipment
test code settings, and equipment logs/service
Application management : Application control–level requests and
transmission of application management information
Personnel management : Professional affiliations, educational details,
language detail, practitioner organization unit, practitioner detail, and staff
identification
Listing 22.6 shows a sample HL7 CDA XML document excerpt.
LISTING 22.6 Sample HL7 CDA XML Document
(Excerpt)
<?xml version=”1.0”?>
<!DOCTYPE levelone PUBLIC “-//HL7//DTD CDA Level
One 1.0//EN” > <levelone>
<clinical_document_header>
<id EX=”a123” RT=”2.16.840.1.113883.3.933”/>
<set_id EX=”B” RT=”2.16.840.1.113883.3.933”/> <version_nbr V=”2”/>
<document_type_cd V=”11488-4”
S=”2.16.840.1.113883.6.1” DN=”Consultation note”/>
<origination_dttm V=”2000-04-07”/>
<confidentiality_cd ID=”CONF1” V=”N”
S=”2.16.840.1.113883.5.1xxx”/> <confidentiality_cd ID=”CONF2” V=”R”
S=”2.16.840.1.113883.5.1xxx”/> <document_relationship>
<document_relationship.type_cd V=”RPLC”/>
<related_document>
<id EX=”a234” RT=”2.16.840.1.113883.3.933”/> <set_id EX=”B”
RT=”2.16.840.1.113883.3.933”/> <version_nbr V=”1”/>
</related_document>
</document_relationship> <fulfills_order>
<fulfills_order.type_cd V=”FLFS”/>
<order><id EX=”x23ABC”
RT=”2.16.840.1.113883.3.933”/></order> <order><id EX=”x42CDE”
RT=”2.16.840.1.113883.3.933”/></order>
</fulfills_order> <patient_encounter>
<id EX=”KPENC1332”
RT=”2.16.840.1.113883.3.933”/> <practice_setting_cd V=”GIM”
S=”2.16.840.1.113883.5.1xxx”
DN=”General internal medicine clinic”/> <encounter_tmr
V=”2000-04-07”/>
<service_location>
<id EX=”KXLPa123” RT=”2.16.840.1.113883.3.933”/> <addr>
<HNR V=”970”/> <STR V=”Post St”/>
<DIR V=”NE”/>
<CTY V=”Alameda”/> <STA V=”CA”/>
<ZIP V=”94501”/> </addr>
</service_location>
</patient_encounter>
</clinical_document_header> <body
confidentiality=”CONF1”>
<section>
<caption>
<caption_cd V=”8684-3” S=”2.16.840.1.113883.6.1”/> History of
Present Illness
</caption>
<paragraph>
<content>
Henry Levin, the 7th is a 67 year old male referred
for further asthma management. Onset of asthma in his teens. He was
hospitalized twice last year, and already twice this year. He has not been able
to be weaned off steroids for the past several months.
</content>
</paragraph>
</section>
<section>
<caption>
<caption_cd V=”1234-X”
S=”2.16.840.1.113883.6.1”/>Plan </caption>
<list>
<item><content>Complete PFTs with lung
volumes.</content></item>
<item><content>Chem-7</content></item>
<item>
<content>
Provide educational material on inhaler usage and
peak flow self-monitoring.
</content>
</item>
<item>
<content>Decrease prednisone to 20qOD
alternating with 18qOD.</content>
</item>
<item><content>Hydrocortisone cream to finger
BID.</content></item> <item><content>RTC 1
week.</content></item>
</list>
</section>
</body>
</levelone>
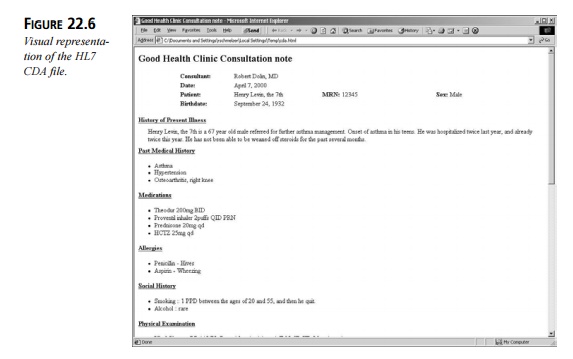
The complete version of this file is shown in a Web browser in Figure
22.6.
Due to HIPAA’s high visibility in the health care arena, HL7 has become
significantly involved with HIPAA implementation as well as legislation. It has
produced an adden-dum to the HIPAA specification to specifically enable certain
aspects of the HIPAA-mandated electronic transmission of patient records.
Future projects will include Home Health, Skilled Nursing Facility, Durable
Medical Equipment (DME), End Stage Renal Disease (ESRD), and Preauthorization
and Referrals.
Related Topics