Chapter: Essentials of Psychiatry: Anxiety Disorders: Generalized Anxiety Disorder
Generalized Anxiety Disorder:Comorbidity with Other Disorders
GAD: Comorbidity with Other Disorders
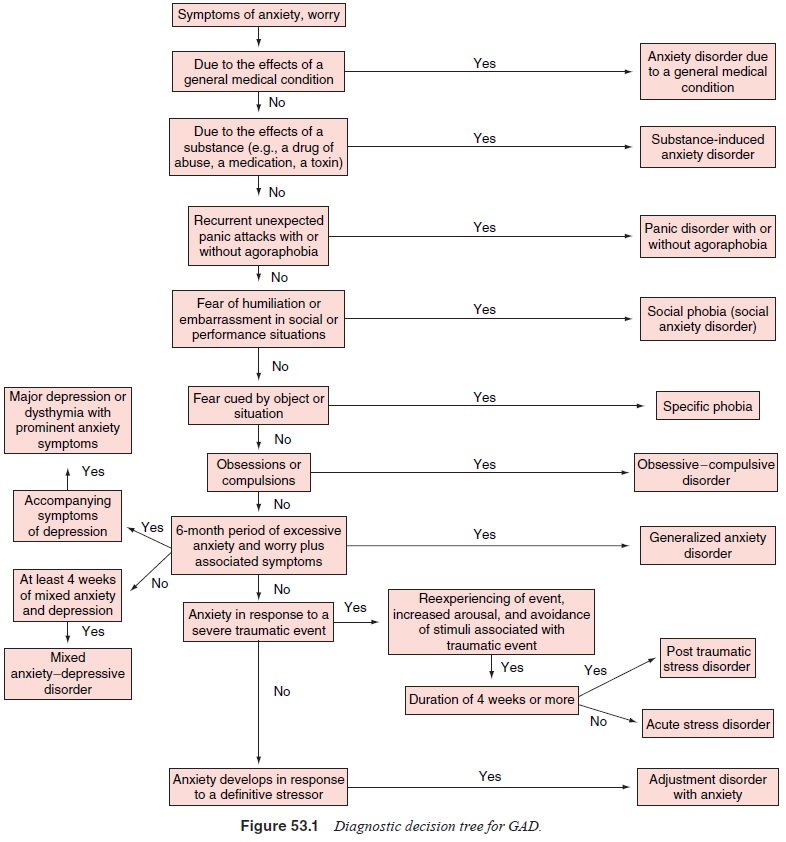
Despite different methodological approaches in early studies, the
available studies report a high prevalence of psychiatric comor-bidity in
patients with GAD. For example, in some studies more than 90% of GAD patients
had additional symptoms that fulfilled criteria for at least one or more
concurrent disorders (range of 45–91%). An examination of the relative
frequencies of various comorbid diagnoses in patients with GAD obtained from
the available studies reveals that other anxiety and mood disorders frequently
complicate the course of GAD (see diagnostic deci-sion tree for GAD: Figure
53.1).
The National Comorbidity Survey showed 90% of re-spondents with lifetime
GAD had at least one other lifetime dis-order and of those with current GAD,
66% had at least one other current disorder. The most common comorbidities
(specifically that criteria for both disorders were met) were found for mood
disorders (major depression and dysthymia), panic disorder and (for current
comorbidity only) agoraphobia. High 12 month rates for comorbidity for GAD and
major depression were reaffirmed in the NCS-R (Kessler et al., 2005). Other studies have also found that the highest
comorbidities were with depressive disor-ders and panic disorders. GAD usually
has an earlier onset than other anxiety and depressive disorders when comorbid
disorders are present. Brawman-Mintzer and associates (1993) found that GAD had
an onset before dysthymia and panic disorder, and af-ter simple and social
phobia. Further, onset of major depression seemed to follow the onset of
anxiety. Similar findings have been reported by other investigators.
As in adult GAD, childhood GAD (or overanxious anxiety disorder as it
was earlier labeled) is also characterized by an unu-sual degree of
comorbidity. Kashani and coworkers (1990) observed that over 50% of children
with overanxious disorder had symptoms that met criteria for at least one
additional psychiatric diagnosis. Among the most prevalent current comorbid
diagnoses are social phobia (16–59%), simple phobia (21–55%), panic disorder
(3–27%) and depression (8–39%). Furthermore, Masi and coworkers (1999) found,
in those children and adolescents they sampled, that 87% had a comorbid
disorder. In particular, high rates of separation anxiety, social anxiety and
depressive disorders were found.
Alcoholism also complicates the clinical course of GAD for some
patients; however, the available literature suggests that the diagnosis of
alcohol abuse is not as prevalent in GAD as in other anxiety disorders, and the
pattern of abuse is often a brief and nonpersistent one. GAD onset is usually
later than that of the alcohol use disorder. Personality disorders have been
observed to co-occur in approximately 50% of patients with GAD. For exam-ple,
rates of GAD and personality disorders in clinical popula-tions have ranged from
31 to 46%. Cluster C personality disorders, specifically avoidant personality
disorder, dependent personality disorder and obsessive–compulsive personality
disorder are com-mon. Interestingly, Cluster A personality traits, in
particular sus-piciousness and mistrust, may be prominent in GAD as well.
Comorbid GAD is associated with increased severity of comorbid disorders
(Kessler, 2000; Kessler et al.,
2005). Ad-ditionally, the presence of comorbid disorders in GAD patients is
related to increased rates of negative outcomes such as dis-ability, impairment
and cost of care. Rates of relapse for GAD patients with comorbid depression
appear higher than in nonco-morbid GAD patients. Further, comorbidity is also
associated with greater treatment seeking. Unsurprisingly, data indicate that
patients with comorbid GAD and depression may have poorer response to treatment
than patients with either disorder only.
Related Topics