Chapter: Essentials of Psychiatry: Anxiety Disorders: Generalized Anxiety Disorder
Generalized Anxiety Disorder: Course, Treatment, Doctor-Patient Relationship
Course
Retrospective and prospective reports indicate that the typical course
of GAD is chronic, nonremitting, and that it often per-sists for a decade or
longer. Rickels and colleagues (1986) re-ported that two-thirds of patients
treated initially with diazepam relapsed within 1 year of discontinuation of
treatment. Other studies utilizing criteria prior to the DSM-III-R for GAD
found comparable levels of chronicity, with almost half the patients re-porting
moderate symptoms at follow-up (Yonkers et
al., 2000).
HARP, a prospective, naturalistic study of 711 adults with DSM-III-R anxiety disorders, recruited initially from psychiat-ric clinics and hospitals in the Boston Metropolitan area, indi-cated that only 15% of those with GAD at baseline experienced a full remission for 2 months or longer at any time during the first year after baseline, and only 25% had a full remission in the 2 years after baseline (Yonkers et al., 1996). Further, among patients who experienced full or partial remission, 27 and 39% respectively, experienced a full relapse during a 3-year follow-up period (Yonkers et al., 2000). Chronicity of GAD was also asso-ciated with cluster B and C personality disorders or a concurrent Axis I comorbidity. Wittchen and coworkers (1994) found that approximately 80% of subjects with GAD reported substantial interference with their life, a high degree of professional help-seeking, and a high prevalence of taking medications because of their GAD symptoms. The disability associated with GAD was found to be similar to that found in individuals with panic disor-der or major depression.
Treatment Approaches
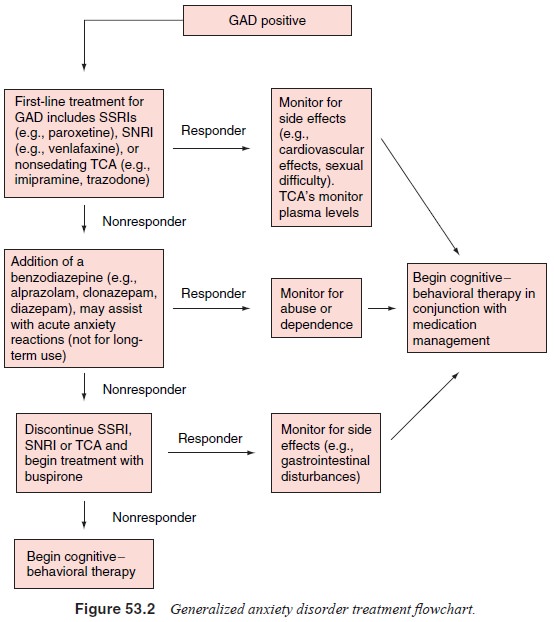
GAD is a chronic, relapsing illness, which means that most treat-ments
do not cure the patient. Furthermore, it also suggests that when treatments are
discontinued, symptoms may return. It fol-lows that a thorough understanding of
the long-term benefits and risks associated with the different treatments
available is impor-tant. Thus, each case must be considered individually
accord-ing to the severity and chronicity of the disorder, the severity of
somatic symptoms, the presence of stressors, and the presence of specific
personality traits. The clinician may also need to work with the patient to
determine how much improvement is suffi-cient. For example, a reduction in
disability may occur without a marked change in symptoms. Symptoms may persist
but oc-cur less frequently, or their intensity may be reduced. All these
variations have important treatment implications, including deci-sions regarding
the need for long-term treatment. Patients with milder forms of GAD may respond
well to simple psychologi-cal interventions, and require no medication
treatment. In more severe forms of GAD, it may become necessary to see the
pa-tient regularly and to provide both more specific psychological and
pharmacological interventions. Figure 53.2 can be used as a guide to the
treatment of GAD.
During the early (acute) phase of treatment, an attempt should be made
to control the patient’s symptomatology. It may take 3 to 6 months for an
optimal response to be achieved. How-ever, there may be a considerable
variation in the length of the initial treatment phase. For example, clinical
response to ben-zodiazepines occurs early in treatment. Response to other
anxi-olytic medications or to cognitive–behavioral treatment gener-ally
requires longer periods of time. During the maintenance phase, treatment gains
are consolidated. Unfortunately, studies suggesting how long treatment should
be continued are limited. Routinely, pharmacological treatment is continued for
a total of 6 to 12 months before attempting to discontinue medications. Recent
data indicate that “maintenance” psychotherapeutic treat-ments such as
cognitive–behavioral therapy may be helpful in maintaining treatment gains in
patients with anxiety disorders following the discontinuation of
pharmacotherapy. It is clear that many patients may experience chronic and
continuous symptoms that require years of long-term treatment.
Doctor–Patient Relationship
The vast majority of patients with GAD who present for treat-ment have
been ill for many years and frequently have received a variety of treatments.
Some patients have been sent to psychia-trists for treatment as a “last resort”
in order to learn how to cope with their various ill-defined somatic and
emotional complaints. Patients may feel shame and guilt over their inability to
control symptoms. They are often demoralized and angry, and feel that their
symptoms are not taken seriously. Thus, it is important to help the patient
understand their illness and to conceptualize it as a health problem rather
than a “personal weakness”. Once the burden of perceived responsibility is
lifted from the patient, and they believe that effective treatment of their
illness is possible, a working alliance with the treating physician can begin.
The treatment plan should be outlined clearly, and the patient cau-tioned that
recovery may have a gradual, variable course. Finally, during the critical
early stages of treatment, the clinician should make a special effort to be
available in person or by phone to answer questions and provide support.
Related Topics