Chapter: Basic Radiology : Radiology of the Breast
Exercise: The Palpable Mass
THE SYMPTOMATIC PATIENT
EXERCISE 5-1.
THE PALPABLE MASS
(Please answer questions for this
exercise before looking at the images, which are presented with the
discussion.)
5-1. In Case 5-1, a 34-year-old woman
who noticed a new lump in her breast, which test
should be ordered first?
A.
Screening mammography
B.
Excisional biopsy
C.
Ultrasonography
D.
Diagnostic mammography
E.
Needle aspiration
5-2. Case 5-2 is a
60-year-old woman who, on the insis-tence of her children, went for her first
routine physi-cal examination in many years. Her doctor found a mass in her
breast. Which test should be ordered first?
A.
Screening mammography
B.
Excisional biopsy
C.
Ultrasonography
D.
Diagnostic mammography
E.
Needle aspiration
5-3. In Case 5-3, a
53-year-old woman thinks she feels a hard nodule deep in her breast. Her
breasts have al-ways been difficult to examine because of their dense nodular
texture. What test should be ordered first?
A.
Screening mammography
B.
Excisional biopsy
C.
Ultrasonography
D.
Diagnostic mammography
E.
Needle aspiration
5-4. In Case 5-4, a
78-year-old woman with a soft, rounded mass discovered during physical
examina-tion, which one of the following statements is true?
A.
A 78-year-old will not likely benefit from mam-mography.
B.
Soft, rounded masses are benign and do not re-quire biopsy.
C.
This mass should initially be aspirated with a needle.
D.
If this mass is carcinoma, the patient will proba-bly die of
this disease.
E. Her physical findings could
easily be caused by a lipoma.
Radiologic Findings
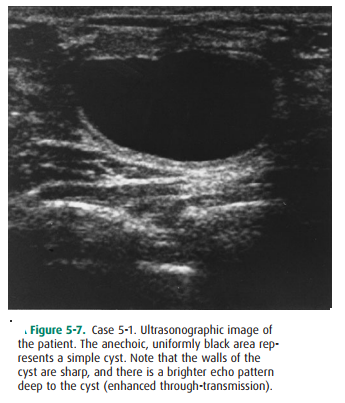
5-1. Ultrasonographic image of the patient in Figure 5-7. The anechoic, uniformly black area represents a simple cyst.
Note that the walls of the cyst are sharp, and there is a brighter echo pattern
deep to the cyst (enhanced through-transmission) (C is the correct answer to
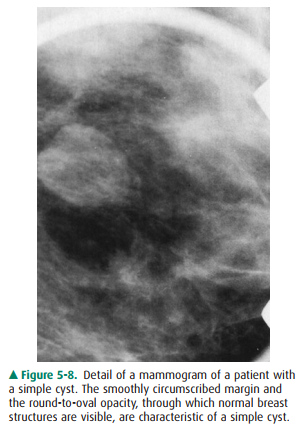
Question 5-1). Figure 5-8 illustrates the mammo-graphic features of a cyst. The
shape is round or oval, and the margins are smooth and sharply delineated.
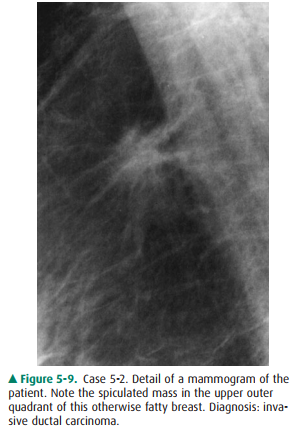
5-2. Detail of a
mammogram (Figure 5-9) of the patient in Case 5-2. Note the spiculated mass in
the upper outer quadrant of this otherwise fatty breast. Diagno-sis: invasive
ductal carcinoma (D is the correct an-swer to Question 5-2).
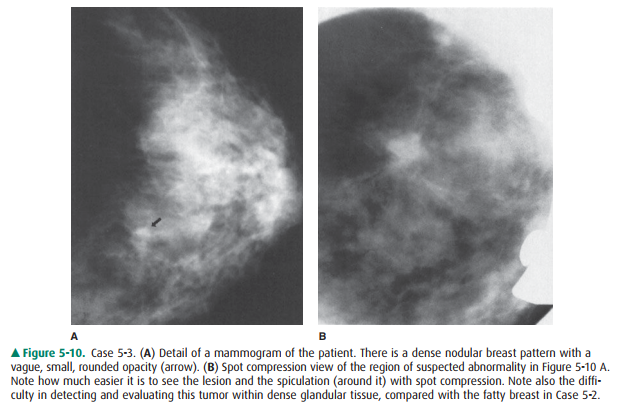
5-3. Detail of a mammogram (Figure 5-10 A) of the pa-tient in
Case 5-3. There is a dense nodular breast pat-tern with a vague, small, rounded
opacity (arrow). Spot compression view (Figure 5-10 B) of the region of
suspected abnormality in Figure 5-10 A. Note how much easier it is to see the
lesion and the spiculation (around it) with spot compression. Note also the
dif-ficulty in detecting and evaluating this tumor within dense glandular
tissue, compared with the fatty breast in Case 5-2 (D is the correct answer to
Question 5-3).
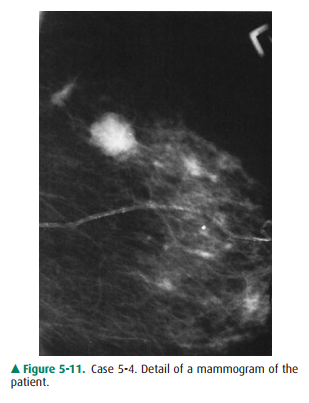
5-4. The 78-year-old
patient in Case 5-4 (Figure 5-11) has a soft mass in her breast and clearly
needs a diagnos-tic mammogram because of her age and the palpable findings (E is
the correct answer to Question 5-4).
Approach to the Palpable Lump
When a breast lump is found,
several questions must be an-swered before proceeding with breast imaging.
First, given that lumpy breasts are a normal variant, when is a lump
sig-nificant? Experts in CBE advise palpation with the flat surface of two to
three fingers, and not with the fingertips. With this technique, nonsignificant
lumps will disperse into back-ground breast density, but a significant lump
will stand out as a dominant mass.
Second, is the lump new or
enlarged? A new lump is more suspicious than a lump that has not changed over a
few years.
Third, how big is the lump? Tiny
pea-sized or smaller lumps, particularly in young women, are often observed
closely with repeated CBE, because small breast nodules are extremely common,
frequently resolve spontaneously, and are usually benign. Repeating CBE in 6
weeks allows for in-terval menses, which frequently causes waning or resolution
of the lump. If the lump persists, diagnostic mammography is indicated.
Fourth, how old is the patient?
If the patient is less than 35 years of age, then radiation is avoided unless
specifically indicated, because the younger breast is more sensitive to
ra-diation. For patients over the age of 35 years, breast imaging begins with a
diagnostic mammogram at the time a lump is deemed to be significant. The
mammogram provides a view of the lump, as well as of the remainder of the involved
breast and the opposite breast, where associated findings may aid in diagnosis
and treatment planning.
If the patient is below 35 years
of age, a significant lump is usually first examined with ultrasonography to
determine whether a simple cyst is present. If there is no cyst, and the
patient is below 30 years of age, the radiologist may choose to obtain a
mammogram, but the density of the breast in such a young patient may limit the
usefulness of radiomammogra-phy, so the mammogram may be limited to one breast
or to a single view.
For women between the ages of 30 and 40 years, judgment is needed as to whether other imaging is indicated. Several factors should be weighed, including age, family history of breast carcinoma, reproductive history, and findings at CBE. If the primary care physician is uncertain of the significance of the findings of CBE, evaluation by a breast specialist may be helpful prior to requesting radiologic tests.
Discussion
The 34-year-old woman in Case 5-1
indeed has a dominant mass, 2 cm in diameter on CBE. She says it was definitely
not present until recently. She has no risk factors for breast can-cer. The
mass most likely is a fibroadenoma or a cyst, but car-cinoma cannot be
excluded. The patient now needs breast ultrasonography.
Ultrasonography is best ordered
before attempted needle aspiration because aspiration can alter the appearance
of simple cysts, giving a misleading suspicious appearance. Therefore, answer
E, needle aspiration, is incorrect.
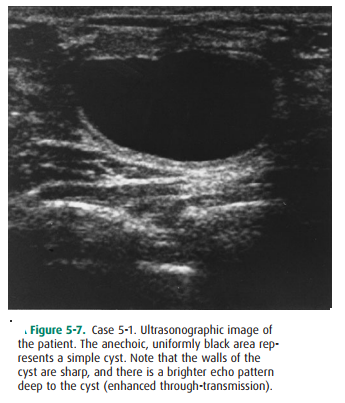
Figure 5-7 shows an image from
the ultrasound study that represents the area precisely in the location of the
pal-pable mass. This area is echo-free, with sharply delineated walls and
posterior acoustic enhancement (increased echogenicity deep to the anechoic
area) consistent with a simple cyst. If these three features are seen, the
probability of a simple cyst is greater than 99% and no further treat-ment is
indicated unless the patient has pain and needs cyst drainage for symptomatic
relief. Therefore, option B, exci-sional biopsy, is inappropriate, because
biopsy can be avoided by showing a simple cyst. No further imaging is needed.
The patient is under the age of 40 years, not yet of screening age, and
radiation should be avoided in young patients. Therefore, answers A and D,
screening and diag-nostic mammography, are not viable options until ultra-sound
is performed.
Simple cysts are very common in
the premenopausal pa-tient and in patients who are being treated with hormone
re-placement therapy. A complex cyst is one that has internal debris—blood,
pus, or tumor. A complex cyst requires fur-ther evaluation, and a short-term
follow-up (6 to 8 weeks) ultrasound may be sufficient. If the debris is due to
attempted aspiration, it may clear on follow-up ultrasonography. Oth-erwise,
excision or needle biopsy is indicated.
The 60-year-old woman in Case 5-2
has a 1.5-cm domi-nant mass on CBE. It is irregular and not freely mobile. The
patient has never had a mammogram. Because she has a pal-pable mass, however, a
screening mammogram is inappro-priate, and option A is incorrect. Although the
mass feels suspicious, she still needs a diagnostic mammogram prior to biopsy
(option B, excisional biopsy, is incorrect), to exclude other lesions such as
multifocal carcinoma. The need for ul-trasonography in a patient of this age is
dictated by the mam-mographic appearance; therefore, option C, ultrasonography,
is incorrect.
Her mammogram (Figure 5-9) shows
a very fatty breast, making any abnormal findings readily apparent. There is a
mass measuring 1 cm in the upper outer quadrant that corresponds to the area of
the palpated mass. The mass is of high density, being white on the mammogram.
There is abundant spiculation and stranding around the mass that is represented
by the radiating linear densities around the pe-riphery of the mass. There is
also retraction of the linear patterns of the normal breast tissue; this
retraction is known as architectural distortion. These findings represent the
classical features of a malignant lesion on mammogra-phy, and this mass must be
biopsied. A spiculated mass such as this is the most common appearance of
invasive breast carcinoma. Less common signs are a circumscribed mass, asymmetric
density, and architectural distortion alone. In-traductal (noninvasive)
carcinoma is more commonly asso-ciated with calcifications.
Spiculation around an invasive
carcinoma corresponds to fingers of tumor, as well as to a desmoplastic
reaction of ad-jacent normal breast tissue responding to the presence of tumor.
This patient has an invasive ductal carcinoma. About 90% of primary breast
carcinomas are ductal carcinomas, and the other 10% are lobular carcinomas.
Besides carcinoma, the primary
differential diagnosis for a spiculated mass includes postsurgical change,
other trauma with hematoma, fat necrosis, infection, and radial scar (a
complex, spontaneous benign lesion involving ductal prolif-eration, elastosis,
and fibrosis).
There are no other lesions in our
patient’s breast, and the other breast appears normal. By mammographic
criteria, then, the patient is a good candidate for treatment with lumpectomy
and radiation therapy rather than mastectomy. Her tumor is solitary, localized
to one quadrant, and her breast tissue is otherwise easy to evaluate
mammographically. Recurrent tumor or additional lesions should, therefore, be
readily seen on posttreatment follow-up mammograms.
For a mass that feels malignant
and appears suspicious on a mammogram, fine-needle aspiration (FNA) at the
bedside may provide a rapid cytological diagnosis of carcinoma. Be-cause FNA
best follows mammography, option E, needle as-piration, is incorrect. FNA may
then be followed by definitive surgical treatment at a later date, after the
patient has had time to consider the treatment options available. If FNA fails
to disclose carcinoma, then excisional biopsy is required be-cause of the
suspicious findings on mammography and CBE. The occasional false-negative FNA
occurs with tumors that do not shed cellular material readily.
Cytology of this palpable mass
revealed ductal carcinoma, and this patient chose to have a lumpectomy.
The 53-year-old patient in Case
5-3 has an ill-defined 1.5-cm hardened nodular area in her breast. Results of
screening mammography less than 1 year ago were normal. Her breast tissue is
not fatty, as in Case 5-2, but she has quite dense, nodular, fibroglandular
tissue, which may ob-scure small masses. The average doubling time of breast
carcinoma makes it unlikely that she has a palpable carci-noma that is entirely
new since her last mammogram. It is quite possible, however, that she has had a
smaller cancer for a few years and that it has now grown large enough to be
palpated. Breast tumors are typically not palpable unless they are at least 1
cm in diameter. Before this stage, in the preclinical phase, the tumor may be
visible up to 2 or 3 years earlier on the mammogram if the breast is fatty. In
dense breasts, as discussed previously, tumors may not be seen on the mammogram
until later stages. For this reason, regular CBE is important. Mammography will
miss some cancers, regardless of the situation, at a rate variably reported to
be between 5% and 15%.
With a new area of abnormality on
physical examina-tion, being in a high-risk age group (over 50 years old), and
having a dense parenchymal pattern, the patient needs another mammogram, this
time a diagnostic mammo-gram of the involved breast only. Option A, screening
mammogram, is incorrect, because it is too soon to repeat screening mammography
at this time and the patient does have a palpable finding—a contraindication
for a screen-ing study.
Figure 5-10 A shows a vague,
rounded opacity within dense fibroglandular tissue. This is in the area of the
palpable mass, as indicated by a small BB placed on the skin over the
abnormality. Detail is not adequate to make a judgment as to the possibility of
malignancy here, or even to confirm that a real lesion is present. The
appearance may merely be due to superimposed normal breast shadows. Compression
spot films are needed to confirm the presence of a mass and to better define
its borders.
Figure 5-10 B shows spot
compression of the questioned opacity seen on initial images. This localized
compression with a smaller paddle placed directly over the abnormality achieves
two things. First, it separates the opacity from adja-cent breast tissue,
demonstrating this to be a discrete mass with high density and not merely
superimposition of normal shadows. Second, it elicits clear spiculation and
architectural distortion around the mass. These features are classic for breast
carcinoma, and biopsy is therefore required. Biopsy of this lesion showed
invasive ductal carcinoma.
The 78-year-old patient in Case
5-4 has a soft mass in her breast and clearly needs a diagnostic mammogram
because of her age and the palpable findings. Soft, rounded masses on physical
examination are often benign fibroadenomata or cysts, but carcinoma may also
present this way (Statement B is false).
Other benign causes of these physical findings include hematoma, abscess, and lipoma (Statement E is true). There-fore, a mammogram may be beneficial for two reasons: (1) if a benign finding is revealed, biopsy may be avoided; and if findings suggest malignancy, optimal treatment can be planned on the basis of extent of the lesion and presence or absence of additional lesions (Statement A is false).
Her mammogram (Figure 5-11) shows
two findings. There is a rounded mass with multiple lobulations and cir-cumscribed
borders. The fact that the borders are not sharply outlined on all sides raises
the suspicion level for this finding. Masses that are sharply delineated may be
followed with serial mammograms at 6-month intervals if they are known not to
be new, are nonpalpable, and show no other features of malignancy. This is not
the case with the patient in Case 5-4. Note the fading margin along portions of
the mass. This mass corresponds to the palpable finding. Ultra-sonography would
be useful to exclude a multiloculated cyst and show the lesion to be solid.
Biopsy is indicated, but nee-dle aspiration without imaging would have been
inappropri-ate (Statement C is false).
A circumscribed mass representing
carcinoma is seen less often than a spiculated mass. About 10% of invasive
ductal carcinomas represent the better-differentiated subtypes, in-cluding
medullary carcinoma, mucinous (colloid) carci-noma, and papillary carcinoma,
all of which are frequently seen as circumscribed masses. They tend to have a
better prognosis than the less well-differentiated garden-variety ductal
carcinomas.
The differential diagnosis for
the circumscribed mass on mammography includes carcinoma (primary as well as
metastatic), fibroadenoma, and cysts; hematoma, abscess, and miscellaneous
benign lesions are seen much less often. Correlation with clinical history and
physical examination can help to narrow the differential diagnosis. When
carci-noma cannot be excluded, either needle aspiration or exci-sional biopsy
is required.
This patient had a needle biopsy.
Because palpation alone could not reliably localize this lesion for needle
biopsy be-cause of its soft nature and the difficulty in fixing its posi-tion,
stereotactic mammographic guidance was used in localizing the lesion for this procedure.
The diagnosis of mu-cinous carcinoma was made by microscopic inspection of the
specimen.
Now, were you astute enough to
perceive the second le-sion? Above and to the left of large mass is a smaller,
dense spiculated mass. This was also biopsied and proved to be a carcinoma of
the very well-differentiated tubular type. Even though the patient has two
lesions now, both carry an excel-lent prognosis and they are unlikely to cause
her death (State-ment D is false). In fact, although mastectomy is certainly a
reasonable treatment for her, local excision would also be an option with these
nonaggressive lesions.
Related Topics