Chapter: Basic Radiology : Radiology of the Breast
Exercise: Lumpiness, Nipple Discharge, and Pain (The Symptomatic Patient)
EXERCISE 5-2.
LUMPINESS, NIPPLE DISCHARGE, AND PAIN
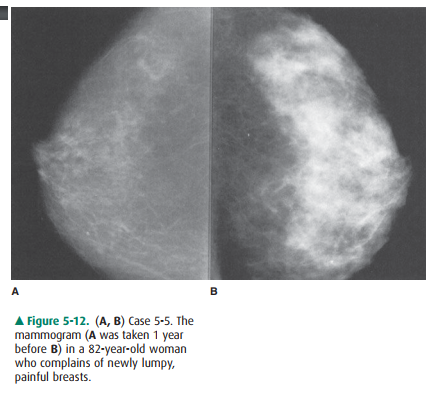
5-5. The most likely explanation for
the patient’s symptoms and mammographic change in Case
5-5 (Figure 5-12) is
A.
hormone effect.
B.
infectious mastitis.
C.
carcinoma.
D.
congestive heart failure.
E.
cystic disease.
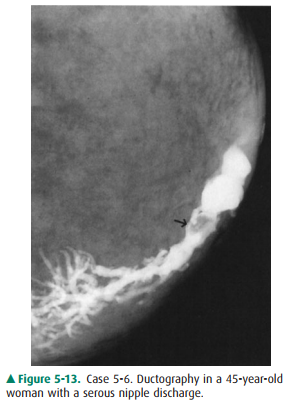
5-6. With respect to
ductography and the condition of the patient in Case 5-6 (Figure 5-13), which
of the fol-lowing statements is true?
A.
Ductography should be performed in all patients with nipple
discharge.
B.
The cause for this patient’s discharge is more likely to be
malignant than benign.
C.
This ductogram shows an extraluminal filling defect.
D.
Ductography has a high specificity for malignant lesions.
E.
Ductography is helpful in guiding the surgeon’s approach.
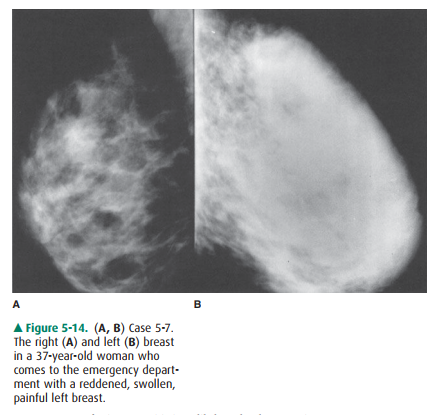
5-7. With respect to
Case 5-7, which of the following statements is false (Figure 5-14)?
A.
There is diffuse abnormality on the left.
B.
Inflammatory carcinoma is high on the differen-tial diagnostic
list.
C.
Infectious mastitis is unlikely to be the cause in this
nonlactating patient.
D.
The mammographic appearance is nonspecific.
E.
Follow-up imaging after a course of antibiotics would be
appropriate.
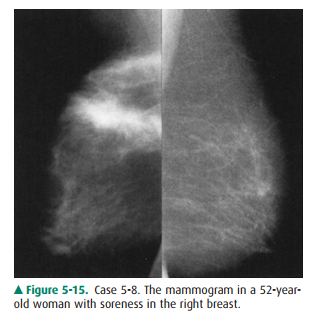
5-8. With respect to
Case 5-8, which one of the following statements is true (Figure 5-15)?
A.
The soreness indicates a benign process.
B.
The appearance is malignant, and biopsy is necessary.
C.
Findings on physical examination and history may radically alter
our management decision.
D.
Bleeding, such as that due to anticoagulation therapy, would not
have this appearance.
E.
The most likely diagnosis is fibrocystic change.
Radiologic Findings
5-5. These mammograms
show a diffuse marked increase in mammographic density with a nodular character
(A is the correct answer to Question 5-5).
5-6. In this ductogram,
contrast has been injected into a portion of a single ductal system with
opacification of the lactiferous sinus and larger branching ducts. Most of the
walls are smooth, as they should be. However, there is a filling defect in one
of the major branches, as exhibited by the lucency outlined by contrast on all
sides and indicated by the arrow (E is the correct answer to Question 5-6;
Statement C is false).
5-7. Mammograms of the
right and left breast show that the entire left breast (B) is abnormally dense
(C is the correct answer to Question 5-7).
5-8. Mammogram shows a
large band of high density with markedly spiculated margins in the upper part
of the breast (C is the correct answer to Question 5-8).
Discussion
Lumpy breasts are a variant of
normal and, as such, require careful physical examination and mammography to
avoid unnecessary surgery, as well as not to miss a carcinoma. Dif-fuse
lumpiness is not a contraindication to screening mam-mography, but when a
particular lump becomes dominant, a diagnostic study is indicated.
The two mammograms of the patient
in Figure 5-12 were obtained 1 year apart. Between these two examinations, the
patient began to exhibit menopause symptoms and was started on hormonal
replacement therapy. The breasts, which were previously largely fatty (A), have
become moderately dense and very lumpy on palpation 1 year later (B). This
change can also be seen, although not usually as dramatically, in the
perimenopausal time of estrogen flare.
Such changes can be seen
asymmetrically or unilaterally, and it is useful to remember the estrogen
effect when evalu-ating mammograms with interval changes. Correlation with
clinical history is then needed.
Answer B, infectious mastitis,
and Answer C, carcinoma, are incorrect as both of these entities are usually
unilateral and focal. Option D, congestive heart failure (CHF), is incor-rect
because CHF causes bilateral changes that have a more linear pattern of
trabecular thickening on mammography, rather than the patchy, ill-defined
nodular pattern character-istic of glandular and cystic densities seen here.
Answer E, cystic disease, is incorrect. Cysts are seen as a component of
hormone-related breast changes, but spontaneous cystic dis-ease alone is rare
at this age.
In the patient in Case 5-6, there
is a single intraluminal filling defect on ductography. However, we cannot
determine from these findings alone whether the defect is due to a be-nign or a
malignant nodule (Statement D is false), although approximately 90% of nipple
discharges are due to benign causes (Statement B is false). The filling defect
in this woman was a benign papilloma, the most common cause of bloody or serous
discharge. Mammograms usually do not show these small, intraductal nodules.
Whether or not a filling defect
is seen on a ductogram, biopsy is needed to rule out carcinoma, and the ductogram
may be helpful in showing the surgeon which area of the breast harbors the
cause of discharge (Statement E is true). However, many surgeons are able to
identify the lobe(s) in-volved in the pathology by inspecting the nipple,
noting the location of the discharging duct, and by palpation, ob-serving which
portion of the breast produces discharge when compressed. Usually, ductography
is not easily per-formed and is of limited usefulness when discharge is not
spontaneous, profuse, and confined to a single duct. There-fore, statement A is
false; ductograms should not be per-formed on all patients with nipple
discharge. Furthermore, only bloody or serous discharges are of concern. A
large portion of patients with discharge have secretions typical of fibrocystic
change (ie, a dark brownish or greenish fluid rather than a truly bloody or
serous discharge). Milky dis-charge is normal.
In Case 5-7, the patient’s entire
left breast is abnormally dense (Statement A is true). There is skin thickening
as well. This is a nonspecific appearance (Statement D is true); infection and
inflammatory carcinoma are both high on the differential diagnosis list (B is
true; C is false). Breast carcinoma may incite an inflammatory response in the
breast, mimicking a benign infectious process both clinically and
radiographically. The patient turns out to have an elevated white blood cell
count and fever with marked pain. This information now makes infection more
likely than tumor, and a course of antibiotics with follow-up imaging to
monitor resolution is appropriate (State-ment E is true).
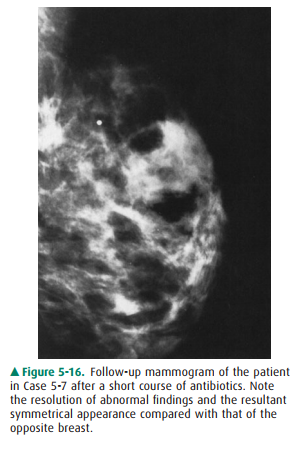
Figure 5-16 shows the follow-up
mammogram after sig-nificant clinical resolution. The mammographic findings
have resolved, and the left breast now appears very similar to the right one.
Infectious mastitis occurs more
frequently in lactating women but is not uncommon in nonlactating women,
particularly in diabetic patients. Imaging (mammography or ultrasound) is
useful to exclude a drainable abscess collec-tion and to provide a baseline for
monitoring resolution to exclude carcinoma.
Case 5-8 illustrates the
importance of correlation with history and physical examination. This patient
has pain, as in the last case, but her mammographic abnormality is much more
localized and appears more like a malignant mass, being a high-density opacity
with excessive spicula-tion. However, this, too, is a benign process. The
patient was in a motor vehicle accident 2 months earlier and sustained a severe
injury to the right side of her chest. Physical exami-nation shows a resolving
laceration and contusion that ex-tends in a linear fashion over the right
breast (no wonder she is sore!). A CT scan performed at the time of trauma
showed the acute injury precisely in the area shown on the mammogram. These
mammographic features are consis-tent with a resolving hematoma from acute
trauma. There-fore, no further action is warranted at this time, other than
follow-up (Statement C is true). Although pain is not a prominent feature of
carcinoma, patients with cancer may be symptomatic. Therefore, pain does not
always indicate benignancy (Statement A is false).
The mammographic appearance would
certainly be highly suspicious for invasive carcinoma in the absence of
clinical information, but with careful correlation we are able to avoid biopsy
in this case (Statement B is false).
Anticoagulation therapy with
resultant bleeding could also have this appearance (Statement D is false).
Fibrocystic change, although very
common, is an unlikely diagnosis. Fibrocystic change appears as increased
cloudy densities, nodular densities, and occasionally some thickened linear
densities, but rarely as a spiculated mass (Statement E is false).
Related Topics