Chapter: Basic Radiology : Radiology of the Breast
Exercise: The First Mammogram(The Asymptomatic Patient)
THE ASYMPTOMATIC PATIENT
EXERCISE 5-3. THE FIRST MAMMOGRAM
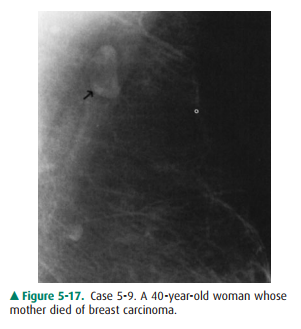
5-9. According to the
American Cancer Society, the best program of breast screening for this woman in
Case 5-9 (Figure 5-17) includes all of the following except
A.
yearly MRI.
B.
yearly mammograms.
C.
cessation of routine mammograms at age 65.
D.
annual clinical breast examination.
5-10. The most likely
diagnosis in Case 5-10 (Figure 5-18) is

A.
complex cyst.
B.
fibroadenolipoma.
C.
galactocele.
D.
ductal carcinoma.
E.
oil cyst.
5-11. The differential
diagnosis in Case 5-11 (Figure 5-19) includes all of the following except
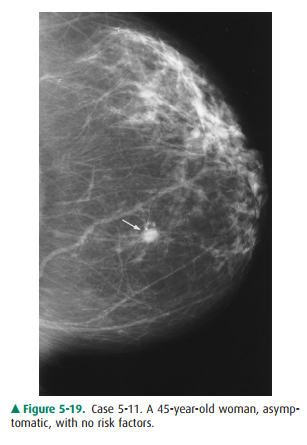
A.
invasive ductal carcinoma.
B.
cyst.
C.
intraductal comedocarcinoma.
D.
fibroadenoma.
E.
mucinous carcinoma.
Radiologic Findings
5-9. Detail of mammogram
of the patient in this case shows a smoothly marginated small mass with a
lucent center (arrow) (C is the correct answer to Question 5-9).
5-10. The mammogram in
this case shows a circumscribed mass (arrows) with internal lucency as well as
opacity (B is the correct answer to Question 5-10).
5-11. Mammogram of
patient in this case shows a nodular density (arrow), with indistinct margins
(C is the correct answer to Question 5-11).
Discussion
In Case 5-9, the 40-year-old
woman has a strong family his-tory of breast cancer, which puts her at high
risk for develop ing the disease. As was stated in the introduction to this
chap-ter, controversy exists concerning when mammographic screening should be initiated
and the appropriate frequency of examinations in different groups. Most experts
agree, however, that patients with a strong family history will bene-fit from
screening beginning at age 40. The American Cancer Society (ACS) recommends
annual screening from age 40 in all female patients; therefore, B is not the
correct answer.
Although the upper age limit for
mammographic screen-ing has not been defined, we certainly cannot recommend
cessation over age 65, because the prevalence of breast cancer is greatest in
women in their 50s and 60s. Current ACS guide-lines recommend yearly mammograms
for all women over the age of 40 years. Appropriate age for termination of
screening is best judged by the patient’s physician, weighing life expectancy
against potential benefits from screening.
ACS recommends annual screening
MRI in women at high risk for breast cancer. ACS also recommends yearly
physical examination by the physician to detect tumors missed by mammography,
as well as those that become de-tectable between routine mammograms (interval
cancers). Therefore, A and D are not correct answers to Question 5-9.
This patient’s mammogram is
normal and demonstrates a typical normal lymph node. The node is smoothly
mar-ginated and has a fatty hilum, indicated by the darker center.
In Case 5-10, there is a
circumscribed mass in the axillary tail of this breast. The key to diagnosis is
the mixture of den-sities within the lesion. There are medium-density opacities
interspersed with lucencies within a smoothly marginated mass. This appearance
is pathognomonic for a fibroadeno-lipoma, sometimes called by the misnomer
hamartoma. Being composed of elements of normal breast (fatty, glandu-lar, and
fibrous tissues) organized within a thin capsule, a fi-broadenolipoma forms a
“breast within a breast.” As such, it is benign and needs no further
evaluation. It may be palpable as a soft mass.
The point to remember here is
that fat-containing masses are always benign. Answer D, ductal carcinoma, is
incorrect. The differential diagnosis of a fatty mass, besides
fibroadenolipoma, includes lymph node, as in Case 5-9, galactocele, lipoma, and
oil cyst. Galactoceles are usually smaller and are most commonly seen in
lactating women (Answer C is incorrect).
Oil cysts result from fat
necrosis and are usually smaller. Typically, they are entirely lucent, as they
are filled with oil, except for a thin wall (Answer E is incorrect).
Option A, complex cyst, is
incorrect because this entity would not contain fat. A cyst, whether it contains
serous fluid, blood, or pus, is always opaque and of low to high den-sity, not
lucent.
In Case 5-11, an asymptomatic
45-year-old woman’s first mammogram shows a 1-cm nodule centrally located in
this breast. The differential diagnosis remains broad without fur-ther studies
to help characterize this nodule. All choices ex-cept option C, intraductal
comedocarcinoma, may have this appearance. Intraductal carcinoma, when not
mammo-graphically occult, usually appears as microcalcifications. Be-cause the
margins are indistinct, however, the patient must be recalled for additional
imaging to rule out carcinoma.
The sonographic image shows a
solid lesion, ruling out a simple cyst. Spot compression is then used to
evaluate the borders. If all margins were to appear smooth, one acceptable
course of action would be serial 6-month follow-up mam-mograms for a period of
2 years to demonstrate stability. If any change occurs during this time, biopsy
is indicated.
Spot compression (Figure 5-20 A)
reveals that portions of the border are not smooth, raising the level of
suspicion for malignancy. To exclude carcinoma, biopsy is needed.
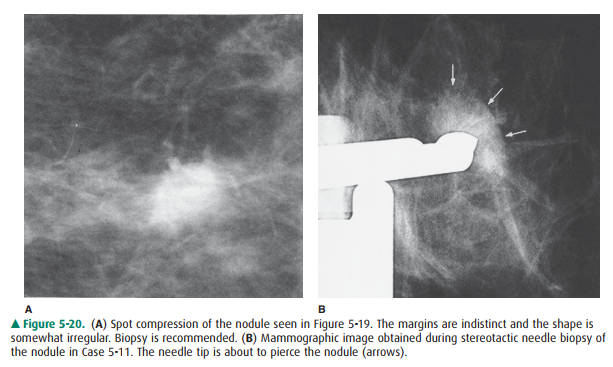
Biopsy may be accomplished with
excision or with needle biopsy. Excision would require needle localization of
the nodule for the surgeon, because this is a nonpalpable lesion. Core needle
biopsy, either stereotactic or ultrasound-guided, is preferable because it is
minimally invasive, causes less mor-bidity to the patient, leaves no distortion
in the breast or on the skin, and is often less expensive than surgical
excision. Accurate needle biopsy devices, however, are expensive and are not
universally available.
This nodule was diagnosed as a
fibroadenoma with stereotactic core needle biopsy (Figure 5-20 B).
Fibroadeno-mas are very common and are frequently the cause of benign breast
biopsy. They occur in very young women (teenagers and women under 30 years of
age) and persist undiscovered through the age at which the first mammogram is
obtained, then, upon discovery, become a concern of both physician and patient.
They may also become palpable or mammo-graphically visible in older women after
previously normal mammograms. They continue to be a management problem, because
fibroadenoma and carcinoma have overlapping mammographic features and both are
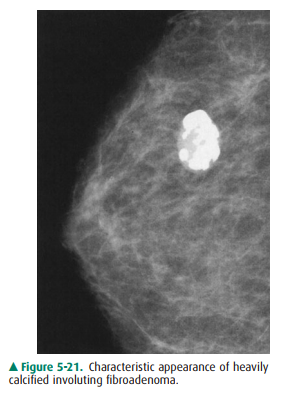
common lesions in middle-aged women. With age, fibroadenomas become invo-luted
and heavily calcified, thereby revealing their true iden-tity (Figure 5-21).
Without this appearance, however, biopsy is often necessary.
A high index of suspicion and careful
evaluation, together with either close follow-up or liberal use of needle
biopsy, are needed to minimize both false-negative impressions and ex-cessive
breast surgery.
Related Topics