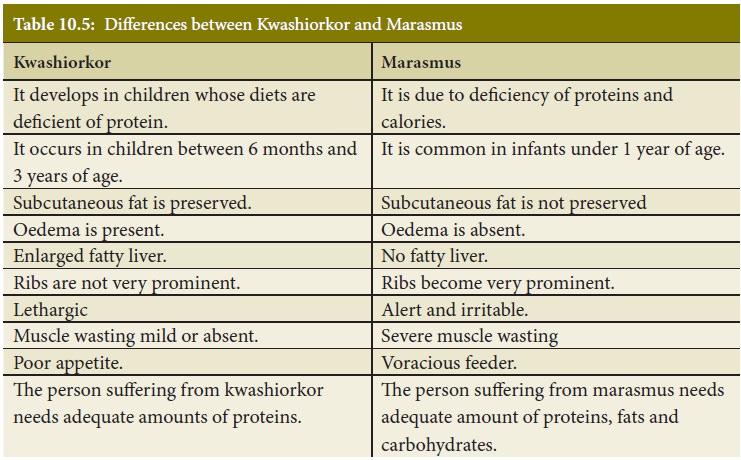
Chapter: 11th Nutrition and Dietetics : Chapter 10 : Proteins and Lipids
Effects of protein deficiency: Protein Energy Malnutrition
Effects
of protein deficiency
Diseases due to the deficiency of proteins
and calories occur commonly among weaned infants and pre-school children in
India and other developing countries.
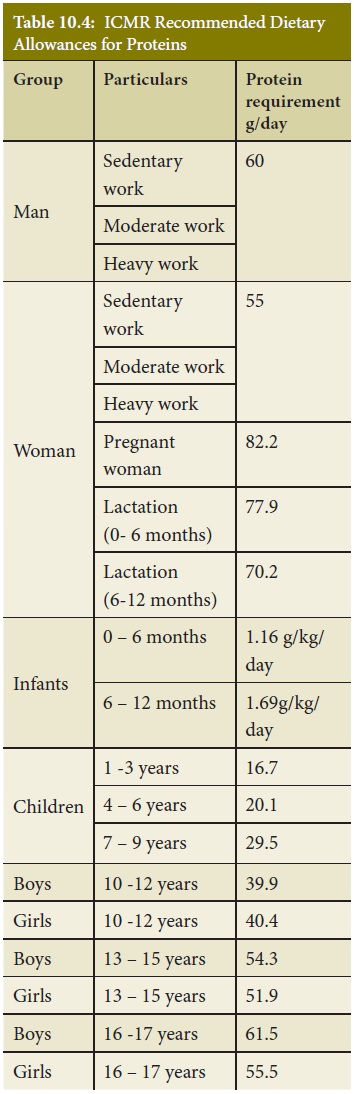
Protein Energy Malnutrition
Protein Energy
Malnutrition (PEM) is defined as a range of pathological conditions arising
from coincident lack of varying proportions of protein and calorie,
Under
nutrition is a complex condition with multiple deficiencies such as
proteins,energy and micro nutrient deficiencies often occurring together. According
to WHO, malnutrition is an underlying factor in over 50 % of the 10 – 11
million yearly deaths of children under 5 years.
Classification of PEM
Protein energy
malnutrition may be classified into three types as follows:
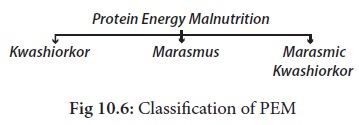
Causes of PEM
PEM is prevalent in
all parts of the World and in all ages. It is primarily a disease that occurs
in young children who live in poverty. In India, PEM is the most widespread
form of malnutrition among pre-school children. A majority of them suffer from
varying grades of malnutrition.
The paths leading from
early weaning to Nutritional marasmus and from protracted breast feeding to
kwashiorkor is schematically presented below:
Clinical signs and symptoms of PEM
I. Kwashiorkor
This disease was first
reported to occur in children in Africa by Dr.Cicely Williams in 1935.

It is caused by
deficiency of proteins in the diet. The important symptoms of the disease are:
·
Growth failure
·
Oedema of the face and lower limbs
·
Muscle wasting
·
Fatty liver
·
Anorexia(loss of appetite)
·
Diarrhoea
·
Change in the colour, sparse, soft and thin hair.
·
Change in the
colour
of
the skin(hypo and
hyperpigmentation)
·
Anaemia
·
Vitamin A deficiency
·
Angular stomatitis(Cracks in the corners of mouth)
·
Cheilosis (inflammation and cracks in lips)
·
Moon face
II. Marasmus
This is caused by
severe deficiency of proteins and calories in the diet. The important features
are as follows:

·
Severe wasting of muscles
·
Loss of subcutaneous fat (Limbs appear as skin and bones)
·
Skin is dry and atrophic
·
Anaemia
·
Eye lesions due to Vitamin A deficiency
·
Irritability and fretfulness
· Diarrhoea
·
Dehydration
·
Body temperature is sub-normal
·
Failure to thrive
·
Wrinkled skin - Old man’s face
·
Grossly underweight
III. Marasmic Kwashiorkor
Children suffering
from this disease show signs of both kwashiorkor and marasmus.
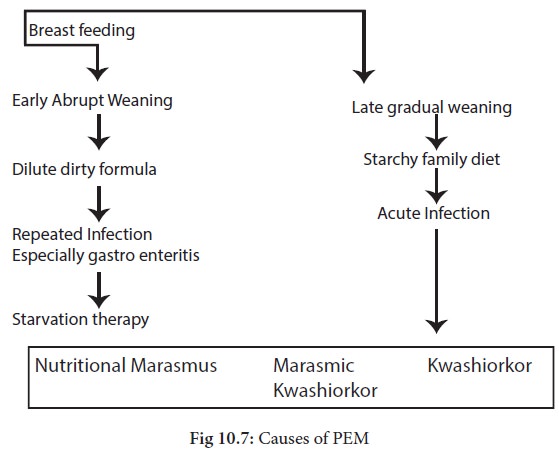
Differences between Kwashiorkor and Marasmus
Treatment of PEM
Children with severe
PEM are often seriously ill when they first present for treatment. They should
be admitted to a hospital for the treatment of life- threatening problems.
Specific deficiencies should be corrected and metabolic abnormalities reversed.
When the child’s condition is stable and the appetite has returned,which is usually
after 2- 7 days ,the treatment can be continued outside the hospital .
A. Hospital based management
Dehydration: Diarrhoea leading to
dehydration is a serious and often fatal event in children with severe
malnutrition. Skin elasticity is poor in children with marasmus and their eyes
are normally sunken. Unlike Kwashiorkor, the altered skin elasticity is masked
by oedema. Patients with mild to moderate dehydration can be treated by oral or
nasogastric administration of fluids.
Infection: Infection is often the
immediate cause of death in PEM. It is difficult to detect infections
clinically as fever and rapid pulse rate may not be present in severely
malnourished patients. Since infection is common, antibiotics should be given
routinely to all malnourished patients. Children with complications should be
treated with broad spectrum antibiotics like amoxicillin and ampicillin.
Intestinal infections like ascariasis mustbetreated with appropriate de-worming
agents.
Hypoglycemia: A child may become
drowsy or develop convulsions due to hypoglycaemia. In mild cases, oral
administration of 50 ml of 10% glucose may be sufficient. If a child develops
convulsions or becomes unconscious, 10% glucose should be given
intravenously(5ml/kg) followed by 50ml of 10% glucose by nasogastric tube,
Hypothermia: Marasmic children are
prone to have low body temperature. If the room is cold, the child should be
properly covered with a blanket. The state of shock should be treated with
intravenous injection of glucose –saline or blood transfusion.
Anaemia: Severe anaemia is
dangerous, as it can result in heart failure. If the haemoglobin falls below
5g/dl,blood transfusion should be given.
B. Dietary management
Although treatment of
complications can reduce mortality, proper dietary management is important for
complete recovery. The child should be given a diet providing sufficient
quantities of calories and protein, in gradually increasing amounts, without
provoking vomiting or diarrhoea. It is best to begin with liquid formula, as it
is easy to feed and measure the intake. Initially the child may refuse the
feeds due to lack of appetite. As the appetite improves and child starts taking
food by mouth,solid supplements can be introduced. The diet should be given
frequently and in small amounts.
High energy intakes (150Kcal/kg) and high protein intakes (3-4g/kg) are required for rapid recovery. Most hospitals use milk-based formulas for feeding malnourished children. Either fresh milk or skimmed milk can be used for preparing the formula. Sugar and vegetable oil are added to increase the energy content. In older children, an entirely liquid diet is not necessary as they can accept solid foods. A mixed cereal-based diet can be given with added oil to increase energy density.
Vitamin and Mineral supplements
Vitamin and mineral
supplements should be given for all malnourished children. Daily supplements of
iron(60mg/ day) and folic acid(1 microgram/day) should be given to correct anaemia along with multivitamin
preparation.
Withthis treatment,
clinical improvement is seen within a week. The child becomes alert and the
appetite improves, Oedema disappears in about 7 -10 days. During this period,
there may be some weight loss, but thereafter, the child starts gaining weight
. After the child is discharged form the hospital, he should be followed up in
the out-patient clinic or at home till he reaches normal weight for height.
Low cost recipes for children recovering from PEM
1. Ragi, green gram,
jaggery: puttu
2. Ragi, Bengal gram,
wheat: puttu
3. Wheat
rava,
green
gram
dhal, vegetable upma
4. Rice, green gram dhal
: pongal / khichdi
5. Rice, bengalgram :
porridge
Related Topics