Chapter: Modern Pharmacology with Clinical Applications: Drugs Used in Asthma
Drugs Used in Asthma
Drugs Used in Asthma
The word asthma is derived from a Greek word meaning difficulty in
breathing. The clinical expression of asthma varies from a mild intermittent
wheeze or cough to severe chronic obstruction that can restrict normal
activity. Acute asthma attacks are triggered by a variety of stimuli, including
exposure to allergens or cold air, exercise, and upper respiratory tract
infections. Recently, a number of genetic polymorphisms have been associated
with an increased risk of developing asthma. Thus, genetic factors probably
contribute to the exaggerated response of the asthmatic airway to various
environmental challenges. The most severe exacerba-tion of asthma, status asthmaticus, is a life-threatening
condition that requires hospitalization and must be treated aggressively. Unlike
most exacerbations of the disease, status asthmaticus is by definition
unresponsive to standard therapy.
The most important outcomes
for successful therapy of asthma are as follows:
·
Prevent chronic and troublesome symptoms
·
Maintain (near) normal pulmonary function
·
Maintain normal activity levels
·
Prevent recurrent exacerbations of asthma and minimize the need for
emergency department visits or hospitalizations
·
Provide optimal pharmacotherapy with mini-mal or no adverse effects
Pathophysiology
Asthma symptoms are produced
by reversible narrow-ing of the airway, which increases resistance to airflow
and consequently reduces the efficiency of movement of air to and from the
alveoli. In addition to airway ob-struction, cardinal features of asthma include
inflamma-tion and hyperreactivity of the airway. In contrast to chronic obstructive pulmonary disease (emphysema
and chronic bronchitis), the airway
obstruction associated with asthma is generally reversible. However, severe
long-standing asthma changes the architecture of the airway. These changes,
including smooth muscle hyper-trophy and bronchofibrosis, can lead to an
irreversible decrement in pulmonary function. These structural changes are
limited to the airways. The lung parenchyma is generally spared.
An aberrant immune response
associated with al-lergy appears to underlie asthma in most children over age 3
years and in most young adults; allergy-induced asthma is also known as extrinsic asthma. In contrast, a large
number of patients, especially those who acquire asthma as older adults, have
no discernible immunolog-ical basis for their condition, although airway
inflamma-tion remains a characteristic of the disease; this type of asthma is
termed intrinsic asthma. Other
patients may have both allergic and nonallergic forms of asthma.
Airway Obstruction
Three factors contribute to
airway obstruction in asthma: (1) contraction of the smooth muscle that
sur-rounds the airways; (2) excessive secretion of mucus and in some, secretion
of thick, tenacious mucus that ad-heres to the walls of the airways; and (3)
edema of the respiratory mucosa. Spasm of the bronchial smooth muscle can occur
rapidly in response to a provocative stimulus and likewise can be reversed
rapidly by drug therapy. In contrast, respiratory mucus accumulation and edema
formation are likely to require more time to develop and are only slowly
reversible.
Airway Inflammation
The recognition that asthma is a disease of airway in-flammation (Fig. 39.1) has fundamentally changed the
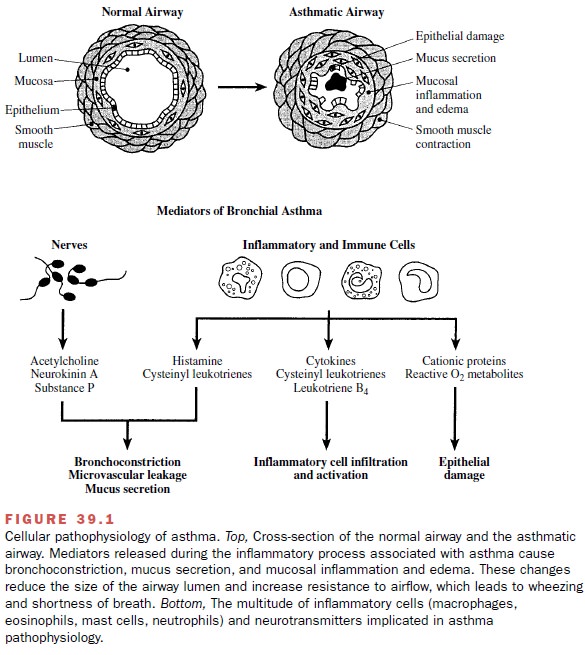
Thus, it is useful to discuss the involvement of various
mediators and in-flammatory cells in antigen-induced asthma, an exten-sively
studied, albeit simplistic, model of the disease. In this model, antigens, such
as ragweed pollen or house mite dust, sensitize individuals by eliciting the
produc-tion of antibodies of the immunoglobulin (Ig) E type. These antibodies
attach themselves to the surface of mast
cells and basophils. If the
individual is reexposed to the same
antigen days to months later, the resulting antigen–antibody reaction on lung
mast cells will trigger the release of histamine
and the cysteinyl leukotrienes,
agents that produce bronchoconstriction, mucus secre-tion, and pulmonary edema.
Mast cells also release a va-riety of chemotactic mediators, such as leukotriene B4 and cytokines. These agents recruit and
activate addi-tional inflammatory cells, particularly eosinophils and alveolar
macrophages, both of which are also rich sources of leukotrienes and cytokines.
Ultimately, re-peated exposure to antigen
establishes a chronic inflam-matory state in the asthmatic airway.
Related Topics