Chapter: Modern Pharmacology with Clinical Applications: Drugs Used in Asthma
Alternative Therapies
ALTERNATIVE
THERAPIES
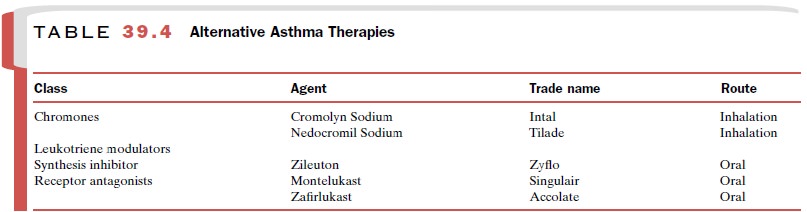
A number of medications
useful in the treatment of asthma are neither strictly bronchodilators nor
antiin-flammatory agents. They are classified as alternative asthma therapies
(Table 39.4). These drugs, used pro-phylactically to decrease the frequency and
severity of asthma attacks, are not indicated for monotherapy. They are used
along with adrenomimetic bronchodilators, corticosteroids, or both.
Leukotriene Modulators
Until the late 1990s, nearly 3 decades had passed since the introduction of a truly new class of antiasthma drugs hav-ing a novel mechanism of action. This situation changed with the introduction of zafirlukast (Accolate) and montelukast (Singulair), cysteinyl leukotriene (CysLT) receptor antagonists, and zileuton (Zyflo), a leukotriene synthesis inhibitor.
CysLTs include leukotrienes C4, D4, and E4. These mediators are
products of arachidonic acid metabolism and make up the components of slow-reacting substance of anaphylaxis.
Basic Pharmacology
The cysteinyl leukotrienes
are generated in mast cells, basophils, macrophages, and eosinophils. These
media-tors have long been suspected of being key participants in the
pathophysiology of asthma. In particular, the powerful bronchoconstrictor
activity of these leuko-trienes has implicated them as major contributors to
the reversible component of airway obstruction. Additional evidence suggests
that their pathophysiologic role ex-tends beyond their ability to elicit
bronchoconstriction. Thus, it is now believed that these substances stimulate
mucus secretion and microvascular leakage, both of which contribute to airway
obstruction. The relative im-portance of the various actions of the cysteinyl
leukotrienes in the complex pathophysiology of asthma is not clear.
The biological actions of the
cysteinyl leukotrienes are mediated via stimulation of CysLT1
receptors. Montelukast and zafirlukast are competitive antagonists of these
receptors. In contrast, zileuton suppresses syn-thesis of the leukotrienes by
inhibiting 5-lipoxygenase, a key enzyme in the bioconversion of arachidonic
acid to the leukotrienes. Zileuton also blocks the production of leukotriene B4,
another arachidonic acid metabolite with proinflammatory activity. The CysLT1-receptor
an-tagonists alter neither the production nor the actions of leukotriene B4.
Clinical Uses
Montelukast, zafirlukast, and zileuton are indicated for the
prophylaxis and chronic treatment of asthma. They should not be used to treat
acute asthmatic episodes. All three agents are
administered orally.
Adverse Effects, Drug Interactions, and Contraindications
Dyspepsia is the most common
side effect of zileuton. Liver transaminase levels are elevated in a small
per-centage of patients taking zileuton. Serum liver transaminase levels should
be monitored and treatment halted if significant elevations occur. Zileuton inhibits the metabolism of theophylline. Thus, when these agents are used concomitantly, the dose of
theophylline should be reduced by approximately one-half, and plasma
con-centrations of theophylline should be monitored closely. Caution should
also be exercised when using zileuton concomitantly with warfarin, terfenadine,
or propranolol, as zileuton inhibits the metabolism of these agents. Zileuton is contraindicated in patients with
acute liver disease and should be
used with caution in patients who
consume substantial quantities of alcohol or have a history of liver disease.
Zafirlukast and montelukast
are well tolerated. Zafirlukast increases plasma concentrations of warfarin and
decreases the concentrations of theophylline and erythromycin. In rare cases,
treatment of patients with CysLT receptor antagonists is associated with the
de-velopment of Churg-Strauss syndrome, a condition marked by acute vasculitis,
eosinophilia, and a worsen-ing of pulmonary symptoms. Because these symptoms
often appear when patients are given the leukotriene receptor antagonists when
they are being weaned from oral corticosteroid therapy, it is not clear whether
they are related to the action of the antagonists or are due to a sudden
reduction in corticosteroid therapy.
Cromolyn Sodium and Nedocromil Sodium
Cromolyn sodium (Intal) and nedocromil sodium (Tilade) are chemically related drugs
called chromones that are used for the prophylaxis of mild or moderate asthma.
Both are administered by inhalation and have very good safety profiles, making
them particularly use-ful in treating children.
Basic Pharmacology
The precise mechanism or
mechanisms whereby cro-molyn sodium and nedocromil sodium exert their
anti-asthmatic activities is unknown. Early work suggested that these agents
act by “stabilizing” mast cells, pre-venting mediator release. However, several
other com-pounds exhibit greater potency for stabilization of mast cells yet
possess no clinical efficacy in asthma. This sug-gests that the therapeutic
activity of cromolyn sodium and nedocromil sodium in asthma is related to one
or more other pharmacological mechanisms. Postulates in-clude inhibitory
effects on irritant receptors, nerves, plasma exudation, and inflammatory cells
in general.
Cromolyn sodium and
nedocromil sodium attenuate bronchospasm induced by various stimuli, including antigen,
exercise, cold dry air, and sulfur dioxide. They suppress inflammatory cell
influx and chemotactic ac-tivity along with antigen-induced bronchial
hyperreac-tivity. Also inhibited is C-fiber sensory nerve activation in animal
models, which may in turn suppress reflex-induced bronchospasm.
Clinical Uses
Cromolyn sodium and nedocromil sodium are used al-most exclusively
for the prophylactic treatment of mild to moderate asthma and should not be
used for the con-trol of acute bronchospasm. These agents are effective in about 60 to 70% of children and adolescents with asthma.
Unfortunately, there is no reliable means to predict which patients will
respond. They are less effec- tive in older patients and in patients with
severe asthma. It may take up to 4 to 6 weeks of treatment for cromolyn sodium
to be effective in chronic asthma, but it is effective after a single dose in
exercise-induced asthma. With respect to clinical efficacy, cromolyn sodium and
nedocromil sodium do not differ in a sub-stantial way.
Adverse Effects
Cromolyn sodium and
nedocromil sodium are the least toxic of available therapies for asthma.
Adverse reac-tions are rare and generally minor. Those occurring in fewer than
1 in 10,000 patients include transient bron-chospasm, cough or wheezing,
dryness of throat, laryn-geal edema, swollen parotid gland, angioedema, joint
swelling and pain, dizziness, dysuria, nausea, headache, nasal congestion,
rash, and urticaria.
Related Topics