Chapter: Modern Pharmacology with Clinical Applications: Drugs Used in Asthma
Adrenomimetic Agents
Adrenomimetic Agents
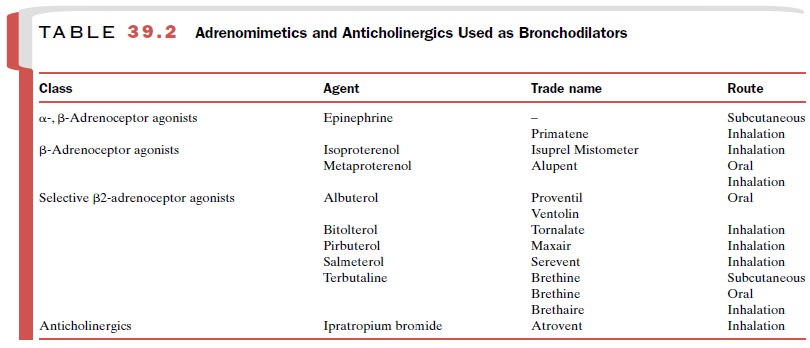
Adrenergic drugs (Table 39.2)
used for the manage-ment of acute and chronic asthma are epinephrine (Primatene), isoproterenol (Isuprel), and a group of adrenoceptor
agonists, including albuterol (Proventil,
Ventolin, Salbutamol), terbutaline (Brethine, Brethaire), and salmeterol (Serevent), that are relatively selective for β2-adrenoceptors . This class of agents has become the mainstay of modern bronchodila-tor therapy. These
agents are used both as needed to re-verse acute episodes of bronchospasm and
prophylacti-cally to maintain airway patency over the long term.
Basic Pharmacology
The principal pharmacological
effects that may be observed in hu-mans treated for bronchospasm are
bronchodilation, tachycardia, anxiety, and tremor. Stimulating β2-adreno-ceptors produces all
of these effects either directly or indirectly.
Epinephrine activates both α - and β-adrenoceptors, whereas isoproterenol is selective for β-adrenoceptors but does not discriminate between β1- and β2-adreno-ceptors. Much-improved selectivity is offered by agents such as albuterol, terbutaline, and salmeterol. These compounds have a higher affinity for β2-adrenoceptors, the predominant subtype in the airway, than for β1-adrenoceptors. Other β2-selective adrenomimetics used as bronchodilators are bitolterol (Tornalate) and pirbuterol (Maxair). Metaproterenol (Alupent), another - adrenomimetic used as a bronchodilator, is less selec-tive for β2-adrenoceptors than is albuterol or terbu-taline.
Epinephrine administered
subcutaneously is used to manage severe acute episodes of bronchospasm and status
asthmaticus. In addition to its bronchodilator ac-tivity through β-adrenoceptor stimulation, a
portion of the therapeutic utility of epinephrine in these acute set-tings may
be due to a reduction in pulmonary edema as a result of pulmonary
vasoconstriction, the latter effect resulting from α-adrenoceptor stimulation.
The effects on pulmonary function are quite rapid, with peak ef-fects occurring
within 5 to 15 minutes. Measurable im-provement in pulmonary function is
maintained for up to 4 hours. The characteristic cardiovascular effects seen at
therapeutic doses of epinephrine include increased heart rate, increased
cardiac output, increased stroke volume, an elevation of systolic pressure and
decrease in diastolic pressure, and a decrease in systemic vascular resistance.
The cardiovascular response to
epinephrine represents the algebraic
sum of both α - and β-adreno-ceptor stimulation. A decrease in diastolic blood pres-sure and a
decrease in systemic vascular resistance are reflections of vasodilation, a β2-adrenoceptor response. The
increase in heart rate and systolic pressure is the re-sult of either a direct
effect of epinephrine on the myo-cardium, primarily a 1 effect, or a
reflex action pro-voked by a decrease in peripheral resistance, mean arterial
pressure, or both. Overt α-adrenoceptor effects, such as systemic vasoconstriction, are not
obvious un-less large doses are used.
Isoproterenol is administered
almost exclusively by inhalation from metered-dose inhalers or from
nebuliz-ers. The response to inhaled isoproterenol and other in-haled
adrenomimetics is instantaneous. The action of isoproterenol is short-lived,
although an objective measurement of pulmonary function has shown an ef-fective
duration of up to 3 hours. When it is adminis-tered by inhalation, the cardiac
effects of isoproterenol are relatively mild, although in some cases a
substantial increase in heart rate occurs.
Terbutaline and albuterol are
administered either orally or by inhalation, whereas salmeterol is given by
inhalation only. All three agents are relatively
selective for β2-adrenoceptors and theoretically are capable of producing
bronchodilation with minimal cardiac stimu-lation. However, the term 2-selectivity is a pharmaco-logical
classification based primarily on the relative po-tency of an individual
adrenomimetic to stimulate the pulmonary or the cardiovascular system. Indeed, β2-agonists invariably produce
a degree of tachycardia at large doses, either by activating sympathetic reflex
pathways as a consequence of systemic vasodilation or by directly stimulating
cardiac β1-adrenoceptors. In ad-dition, a significant number of β2-adrenoceptors are present in
the human heart, and stimulation of these re-ceptors may contribute to the
cardiac effects of β2-adrenoceptor agonists.
Inhaled salmeterol has a
pharmacological half-life in excess of 12 hours, much longer than either
albuterol or terbutaline. The likely basis for this long half-life is that the
long lipophilic tail of salmeterol promotes retention of the molecule in the
cell membrane. Its long duration of action makes salmeterol particularly
suitable for pro-phylactic use, such as in preventing nocturnal symptoms of
asthma. Because of its relatively slow onset of action, salmeterol should not be used to treat acute symptoms.
The second messenger, cyclic
adenosine monophos-phate (cAMP), is thought to mediate the bronchodila-tor
effects of the adrenomimetics. Adrenomimetics en-hance the production of cAMP
by activating adenylyl cyclase, the enzyme that converts adenosine
triphos-phate (ATP) to cAMP. This process
is triggered by the interaction of
the adrenomimetics with β2-adrenoceptors
on airway smooth muscle.
Clinical Uses
Epinephrine is used in a
variety of clinical situations, and although concern has been expressed about
the use of epinephrine in asthma, it is still used extensively for the
management of acute attacks.
Isoproterenol is used principally
by inhalation for the management of bronchospasm. It is also used
intra-venously for asthma and as a stimulant in cardiac arrest.
Terbutaline, albuterol,
salmeterol and other β2-adrenoceptor agonists are used primarily in the man-agement of asthma.
Terbutaline and albuterol have very rapid onset of action and are indicated for
acute symp-tom relief. Salmeterol, in contrast, has a slow onset of action but
a long duration of action. Salmeterol is thus used as prophylactic therapy
only, not to reverse acute symptoms.
In addition to its use as a
bronchodilator, terbutaline is used extensively to control premature labor,
since contractions of uterine smooth muscle are abolished by adrenomimetics .
Adverse Effects
Patients treated with
recommended dosages of epi-nephrine will complain of feeling nervous or
anxious. Some will have tremor of the hand or upper extremity and many will
complain of palpitations. Epinephrine is dangerous if recommended dosages are
exceeded or if the drug is used in patients with coronary artery disease,
arrhythmias, or hypertension. The inappropriate use of epinephrine has resulted
in extreme hypertension and cerebrovascular accidents, pulmonary edema, angina,
and ventricular arrhythmias, including ventricular fibril-lation.
At recommended dosages,
adverse effects from in-haled isoproterenol are infrequent and not serious.
When excessive dosages are used, tachycardia, dizzi-ness, and nervousness may
occur, and some patients may have arrhythmias.
The limiting side effect associated
with orally ad-ministered β2-adrenoceptor agonists is muscle
tremor, which results from a direct stimulation of β2-adreno-ceptors in skeletal
muscle. This effect is most notable on the initiation of therapy and gradually
improves on con-tinued use. β2-Agonists also cause tachycardia and pal-pitations in some
patients. When used by intravenous infusion for premature labor, β2-agonists have been reported
to produce tachycardia and pulmonary edema in the mother and hypoglycemia in
the baby. When ad-ministered by inhalation, the β2-agonists produce only minor side effects.
A few epidemiological studies
suggest that the over-use of β-adrenoceptor agonists is associated with an overall deterioration
in disease control and a slight in-crease in asthma mortality. This apparent
trend may be caused by several factors, the most likely of which is that
patients rely too heavily on bronchodilator therapy to control acute symptoms
at the expense of antiinflam-matory therapy to control the underlying disease process.
Related Topics