Chapter: Modern Pharmacology with Clinical Applications: Drugs Used in Asthma
Antiinflammatory Agents
ANTIINFLAMMATORY
AGENTS
The medical and scientific
communities have recog-nized that asthma
is not simply a disease marked by acute
bronchospasm but rather a complex chronic in-flammatory disorder of the
airways. On the basis of this knowledge,
antiinflammatory agents, particularly corti-costeroids, are now included in the
treatment regimens of an ever-increasing proportion of asthmatic patients.
Corticosteroids
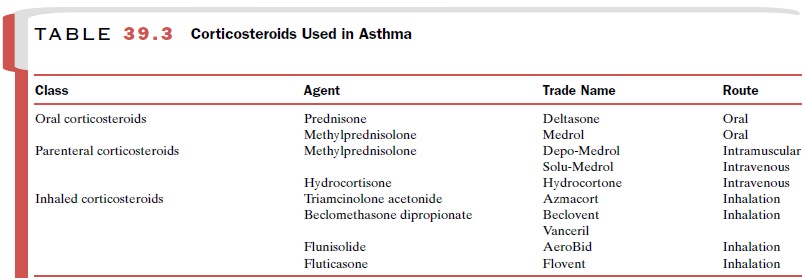
A major breakthrough in
asthma therapy was the intro-duction in the 1970s of aerosol corticosteroids. These agents (Table 39.3) maintain much of
the impressive therapeutic efficacy of parenteral and oral cortico-steroids,
but by virtue of their local administration and markedly reduced systemic
absorption, they are associ-ated with a greatly reduced incidence and severity
of side effects. The success of inhaled steroids has led to a substantial
reduction in the use of systemic cortico-steroids. Inhaled corticosteroids, along with β2-adreno-ceptor agonists, are
front-line therapy of chronic asthma.
Basic Pharmacology
All corticosteroids have the
same general mechanism of action; they traverse cell membranes and bind to a
spe-cific cytoplasmic receptor. The steroid-receptor complex translocates to
the cell nucleus, where it attaches to nu-clear binding sites and initiates
synthesis of messenger ri-bonucleic acid (mRNA). The novel proteins that are
formed may exert a variety of effects on cellular func-tions. The precise
mechanisms whereby the cortico-steroids exert their therapeutic benefit in asthma
remain unclear, although the benefit is likely to be due to several actions
rather than one specific action and is related to their ability to inhibit
inflammatory processes.At the mo-lecular level, corticosteroids regulate the
transcription of a number of genes, including those for several cytokines.
The corticosteroids have an
array of actions in sev-eral systems that may be relevant to their
effectiveness in asthma. These include inhibition of cytokine and mediator
release, attenuation of mucus secretion, up-regulation of β-adrenoceptor numbers,
inhibition of IgE synthesis, attenuation of eicosanoid generation, de-creased
microvascular permeability, and suppression of inflammatory cell influx and
inflammatory processes. The effects of the steroids take several hours to days
to develop, so they cannot be used for quick relief of acute episodes of
bronchospasm.
Clinical Uses
The corticosteroids are
effective in most children and adults with asthma. They are beneficial for the
treat-ment of both acute and chronic aspects of the disease. Inhaled
corticosteroids, including triamcinolone ace-tonide (Azmacort), beclomethasone dipropionate (Beclo-vent, Vanceril), flunisolide (AeroBid), and fluticasone (Flovent), are indicated for maintenance
treatment of asthma as prophylactic therapy. Inhaled corticosteroids are
not effective for relief of acute episodes of severe bronchospasm. Systemic
corticosteroids, including pred-nisone and prednisolone, are used for the
short-term treatment of asthma exacerbations that do not respond to β2-adrenoceptor agonists and
aerosol corticosteroids. Systemic corticosteroids, along with other treatments,
are also used to control status asthmaticus. Because of the side effects
produced by systemically administered corticosteroids, they should not be used
for maintenance therapy unless all other treatment options have been exhausted.
A fixed combination of
inhaled fluticasone and sal-meterol (Advair)
is available for maintenance antiin-flammatory and bronchodilator treatment of
asthma.
Adverse Effects and Contraindications
The side effects of
corticosteroids range from minor to severe and life threatening. The nature and
severity of
side effects depend on the
route, dose, and frequency of administration, as well as the specific agent
used. Side effects are much more prevalent with systemic adminis-tration than
with inhalant administration. The potential consequences of systemic
administration of the corti-costeroids include adrenal suppression, cushingoid
changes, growth retardation, cataracts, osteoporosis, CNS effects and
behavioral disturbances, and increased susceptibility to infection. The
severity of all of these side effects can be reduced markedly by alternate-day
therapy.
Inhaled corticosteroids are
generally well tolerated. In contrast to systemically administered
corticosteroids, inhaled agents are either poorly absorbed or rapidly
metabolized and inactivated and thus have greatly di-minished systemic effects
relative to oral agents. The most frequent side effects are local; they include
oral candidiasis, dysphonia, sore throat and throat irritation, and coughing.
Special delivery systems (e.g., devices with spacers) can minimize these side
effects. Some studies have associated slowing of growth in children with the
use of high-dose inhaled corticosteroids, al-though the results are
controversial. Regardless, the purported effect is small and is likely
outweighed by the benefit of control of the symptoms of asthma.
Care should be taken in
transferring patients from systemic to aerosol corticosteroids, as deaths due
to ad-renal insufficiency have been reported. In addition, al-lergic
conditions, such as rhinitis, conjunctivitis, and eczema, previously controlled
by systemic corticos-teroids, may be unmasked when asthmatic patients are
switched from systemic to inhaled corticosteroids. Caution should be exercised
when taking cortico-steroids during pregnancy, as glucocorticoids are
terato-genic. Systemic corticosteroids are contraindicated in patients with
systemic fungal infections.
Related Topics