Chapter: 11th 12th std standard Class Nursing Health Care Hospital Hygiene Higher secondary school College Notes
Diet In Diseases Of Liver
DIET IN DISEASES OF LIVER
The liver has the most varied and extensive function and is one of the
most important organs involved in the metabolism of food. Most of the end
products of digestion are transported directly to the liver where they are
stored or resynthesized into other forms.
FUNCTIONS OF LIVER
1.
Protein metabolism - synthesis of plasma
proteins, deaminisation of amino acids, the resultant ammonia is detoxified by
conversion to urea. Transamination of amino acids to maintain normal blood
levels of non essential amino acids synthesis of prothrombin / fibrinogen.
2.
Carbohydrate metabolism - synthesis, storage and
release of glycogen. Glycogen is converted to glucose when needed
(glycogenolysis). Liver cells convert protein to glucose to give energy (gluconeogenesis),
synthesis of heparin.
3.
Lipid metabolism - synthesis of lipoproteins,
phospholipids, cholesterol, formation of bile, oxidation of fatty acids.
4.
Mineral metabolism - Iron and copper, both
essential to hemoglobin formation are stored in the liver.
5.
Vitamin metabolism - All fat soluble vitamins
A,D,E,K, as well as ascorbic acid and B-Complex vitamins are stored in the
liver. Carotene is converted to vitamin A and vitamin K to prothrombin.
6.
Drugs are metabolized and hormones are
deactivated in the liver.
Liver
detoxifies chemicals, poisons or drugs entering the body through foods.
AGENTS WHICH CAUSE
DAMAGE TO THE LIVER
Dietary deficiencies
1.
A low protein intake and reduced capacity to
secrete beta lipoproteins as seen in kwashiorkor cause fatty changes in the
liver.
2.
Fatty changes in the liver are also common in
uncontrolled diabetes, in starvation, and obesity. These changes are
reversible.
Infective agents
1.
Virus can cause infection and damage to the
liver. Hepatitis A virus is excreted in the stools and spread by the faecal -
oral route. The patient suffers from jaundice and the liver is enlarged and
tender.
2.
Improperly sterilized needles used in blood
transfusion can transmit Hepatits B virus which causes homologous serum
jaundice.
Toxic agents
1.
Alcohol : Consumption of alcohol produces acute
liver damage and jaundice.
2.
Drugs and Chemicals : Drugs like paracetamol may
damage the liver. Excess stores of iron, copper, galactose and glycogen may
accumulate in the liver and lead to cirrhosis.
JAUNDICE - SYMPTOM OF
LIVER DISORDERS
Jaundice
is a symptom common to many diseases of the liver and biliary tract and
consists of a yellow pigmentation of the skin and body tissues because of
accumulation of bile pigments in the blood.
Jaundice may be produced
due to the following factors / reasons
1.
Obstructive jaundice results from the
interference of the flow of bile by the formation of stone and tumors.
2.
Hemolytic jaundice results from an abnormally
large destruction of blood cells as in pernicious anemia.
3.
Toxic jaundice originates from poisons, drugs or
virus infection.
INFECTIVE HEPATITIS -
SYMPT OMS AND DIETARY MANAGEMENT
Infective
hepatitis is otherwise known as viral hepatitis.
Symptoms : Anorexia, fever, headache, rapid weight loss, loss of muscle tone and abdominal discomfort precede the
development of jaundice. Neglected viral hepatitis leads to cirrhosis of liver.
Treatment consists of adequate rest, nutritious diet and avoidance of further
damage to the liver.
Dietary Management : The objectives of dietary treatment
are to aid in the regeneration of liver tissue and prevent further liver
damage.
A high protein, high carbohydrate, moderate fat is recommended. Small
attractive meals at regular intervals are better tolerated. Over feeding should
be avoided.
Energy : Sufficient calories should be given to maintain weight and reduce protein catabolism. A diet
which supplies 1600 k cals to 2000 k cals is suggested.
Proteins : 1 g
protein per kilogram of body weight daily is needed to overcome negative nitrogen balance, for liver cells to
regenerate and prevent fatty infiltration of the liver. With severe jaundice 40
g and in mild jaundice 60 - 80 g of protein is permitted. In hepatic coma
protein containing foods are avoided and high carbohydrate containing foods are
given.
Fats : In severe jaundice 20 g and moderate jaundice 20-30 g is given. Fat needs to be restricted
when there is obstruction to bile flow and in hepatic coma when fats are not
metabolized by the liver.
Carbohydrates : High intake of carbohydrate is essential to supply enough calories so that tissue proteins are not broken down
for energy. Fruits, fruit juices, vegetable juices, sugar, jaggery and honey
are given to supply adequate electrolytes.
Vitamins : Vitamins are essential to regenerate liver cells. 500 mg of vitamin C, 10 mg of vitamin K, and B-complex vitamins
are essential to meet the daily needs. If anorexia, nausea or vomiting are
present, the vitamins may be given by injection.
Minerals : Oral
feeds of fruit juice, vegetable and meat soups with added salt given orally or through a naso gastric tube help
in maintaining the electrolyte balance.
Foods to be included and avoided are
presented in List.
List
: Foods that can be included and avoided in Infective Hepatitis
Foods
to be included :
Cereal porridge, soft chapathis, bread,
rice, skimmed milk, potato, yam, fruit, fruit juices, sugar, honey, soft
biscuits, custards without butter, and cream.
Foods
to be avoided :
Pulses, beans, meat, fish, chicken, egg,
sweets with ghee, butter or oil, bakery products, dried nuts and fruits,
alcoholic preparation, whole milk and cream.
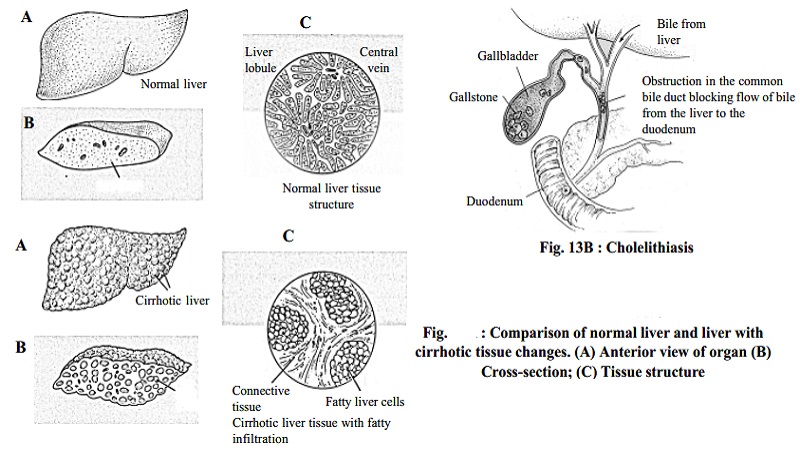
DIETARY MANAGEMENT IN CIRRHOSIS OF LIVER
Cirrhosis
is a condition in which there is destruction of the liver cell due to necrosis, fatty infiltration and fibrosis. It is a serious and
irreversible disease. It occurs after years of excessive alcohol intake in
individuals whose diets are deficient in nutrients. Malnutrition aggravates
injury to the liver and can lead to child hood cirrhosis seen between the age
of 1 to 3 years.
Symptoms
The onset of cirrhosis may be gradual with
gastrointestinal disturbances such as anorexia, nausea, vomiting and pain. The
patient may suffer from weakness, muscle cramps, weight loss and fever. As the
disease progresses jaundice occurs. Ascites which is the accumulation of
abnormal amounts of fluid in the abdomen develops.
Principles of diet
A high calorie, high protein, high carbohydrate, moderate or restricted
fat, high vitamin diet helps in the regeneration of liver and helps to prevent
the formation of ascites. Low fat with supplementation of fat soluble vitamins
and minerals should be given. Sodium should be restricted only when there is
ascites. The diet should be attractive and palatable.
Dietary management
Energy : Since anorexia and ascites are present consumption of food is difficult. A highly nutritious high calorie diet is
necessary because of prolonged undernourishment. The calorie requirement should
be between 2000 - 2500 k cals.
Proteins : A high protein diet is helpful for regeneration of the liver. It also helps to compensate for the considerable loss
of albumin in the ascitic Fluid. In the absence of hepatic coma, a high protein
intake of 1.2 g/kg of body weight is recommended. The protein content of the
diet varies according to the symptoms.
Fats : About 20 g of fat is given provided adequate amounts of protein is supplied.
Carbohydrates : Carbohydrates should be supplied liberally so that the liver may store glycogen. Liver function improves when
an adequate store of glycogen is present.
Vitamins and Minerals : The liver is the major site of storage and conversion of vitamins into their metabolically active form.
In cirrhosis the liver concentration of folate, riboflavin, nicotinamide,
vitamin B12 and vitamin A are decreased.
Vitamin supplementation especially of B vitamins
is required to prevent anaemia. Choline and methionine are useful if fatty
infiltration is present.
Sodium is restricted to 400-800 mg/day in oedema
and ascites. If there is no ascites very little salt is permitted to make the
food more appetizing. Potassium salt is given for ascites and oedema to prevent
hypokalemia.
Iron supplementation is essential as anaemia is
common. A daily dose of 0.3 g of ferrous sulphate tablet 3 times after meals
would also be beneficial. Folic acid 1 mg / day orally is given to treat
macrocytic anaemia.
CHOLECYSTITIS AND CHOLELITHIASIS - DIETARY MANAGEMENT
Cholecystitis is an inflammation of the gall bladder and cholelithiasis
is the formation of gall stones. Inflammation of the gall bladder results from
a low grade chronic infection and may occur with or without gall stones. Gall
stones are of two main groups: Cholesterol and pigment stones.
When inflammation and / or stones are present in the gallbladder, fat in
the diet is the main cause for contraction which causes pain. Surgical removal
is usually indicated if the patient suffers from acute cholecystitis or
cholelithiasis. Intake of fat should be greatly reduced to 20g day and energy
should be derived from carbohydrate.
Cereals in
a soft form, cooked rice, chapathi, bread and idli, milk pudding, curds, cooked
vegetables, kichidi and porridge can be included in the diet. Pulses, beans,
meat, fruit, fruit juices, fish, soft cooked eggs can also be given. These are
high caloric, high protein foods which help in regeneration of liver cells.
Related Topics