Chapter: Medical Physiology: Rhythmical Excitation of the Heart
Control of Excitation and Conduction in the Heart
Control of Excitation and Conduction in the Heart
The Sinus Node as the Pacemaker of the Heart
In the discussion thus far of the genesis and transmis-sion of the cardiac impulse through the heart, we have noted that the impulse normally arises in the sinus node. In some abnormal conditions, this is not the case. A few other parts of the heart can exhibit intrinsic rhythmical excitation in the same way that the sinus nodal fibers do; this is particularly true of the A-V nodal and Purkinje fibers.
The A-V nodal fibers, when not stimulated from some outside source, discharge at an intrinsic rhyth-mical rate of 40 to 60 times per minute, and the Purk-inje fibers discharge at a rate somewhere between 15 and 40 times per minute. These rates are in contrast to the normal rate of the sinus node of 70 to 80 times per minute.
The question we must ask is: Why does the sinus node rather than the A-V node or the Purkinje fibers control the heart’s rhythmicity? The answer derives from the fact that the discharge rate of the sinus node is considerably faster than the natural self-excitatory discharge rate of either the A-V node or the Purkinje fibers. Each time the sinus node discharges, its impulse is conducted into both the A-V node and the Purkinje fibers, also discharging their excitable membranes. But the sinus node discharges again before either the A-V node or the Purkinje fibers can reach their own thresh-olds for self-excitation. Therefore, the new impulse from the sinus node discharges both the A-V node and the Purkinje fibers before self-excitation can occur in either of these.
Thus, the sinus node controls the beat of the heart because its rate of rhythmical discharge is faster than that of any other part of the heart. Therefore, the sinus node is virtually always the pacemaker of the normal heart.
Abnormal Pacemakers—“Ectopic” Pacemaker. Occasionallysome other part of the heart develops a rhythmical dis-charge rate that is more rapid than that of the sinus node. For instance, this sometimes occurs in the A-V node or in the Purkinje fibers when one of these becomes abnormal. In either case, the pacemaker of the heart shifts from the sinus node to the A-V node or to the excited Purkinje fibers. Under rarer condi-tions, a place in the atrial or ventricular muscle devel-ops excessive excitability and becomes the pacemaker.
A pacemaker elsewhere than the sinus node is called an “ectopic” pacemaker. An ectopic pacemaker causes an abnormal sequence of contraction of the different parts of the heart and can cause significant debility of heart pumping.
Another cause of shift of the pacemaker is blockage of transmission of the cardiac impulse from the sinus node to the other parts of the heart. The new pace-maker then occurs most frequently at the A-V node or in the penetrating portion of the A-V bundle on the way to the ventricles.
When A-V block occurs—that is, when the cardiac impulse fails to pass from the atria into the ventricles through the A-V nodal and bundle system—the atria continue to beat at the normal rate of rhythm of the sinus node, while a new pacemaker usually develops in the Purkinje system of the ventricles and drives the ventricular muscle at a new rate somewhere between 15 and 40 beats per minute. After sudden A-V bundle block, the Purkinje system does not begin to emit its intrinsic rhythmical impulses until 5 to 20 seconds later because, before the blockage, the Purkinje fibers had been “overdriven” by the rapid sinus impulses and, consequently, are in a suppressed state. During these 5 to 20 seconds, the ventricles fail to pump blood, and the person faints after the first 4 to 5 seconds because of lack of blood flow to the brain. This delayed pickup of the heartbeat is called Stokes-Adams syndrome. If the delay period is too long, it can lead to death.
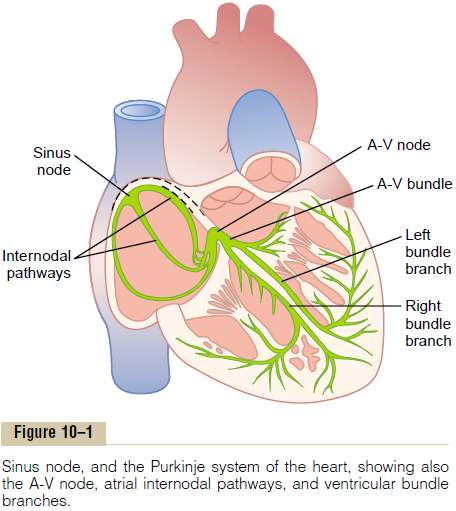
Role of the Purkinje System in Causing Synchronous Contraction of the Ventricular Muscle
It is clear from our description of the Purkinje system that normally the cardiac impulse arrives at almost all portions of the ventricles within a narrow span of time, exciting the first ventricular muscle fiber only 0.03 to0.06 second ahead of excitation of the last ventricularmuscle fiber. This causes all portions of the ventricular muscle in both ventricles to begin contracting at almost the same time and then to continue contract-ing for about another 0.3 second.
Effective pumping by the two ventricular chambers requires this synchronous type of contraction. If the cardiac impulse should travel through the ventricles slowly, much of the ventricular mass would contract before contraction of the remainder, in which case the overall pumping effect would be greatly depressed. Indeed, in some types of cardiac debilities, slow trans-mission does occur, and the pumping effectiveness of the ventricles is decreased as much as 20 to 30 per cent.
Control of Heart Rhythmicity and Impulse Conduction by the Cardiac Nerves: The Sympathetic and Parasympathetic Nerves
The heart is supplied with both sympathetic and parasympathetic nerves. The parasympathetic nerves (the vagi) are distributed mainly to the S-A and A-V nodes, to a lesser extent to the muscle of the two atria, and very little directly to the ventricular muscle. The sympa-thetic nerves, conversely, are distributed to all parts of the heart, with strong representation to the ventricu-lar muscle as well as to all the other areas.
Parasympathetic (Vagal) Stimulation Can Slow or Even Block Cardiac Rhythm and Conduction—“Ventricular Escape.”
Stimulation of the parasympathetic nerves to the heart (the vagi) causes the hormone acetylcholine to be released at the vagal endings. This hormone has two major effects on the heart. First, it decreases the rate of rhythm of the sinus node, and second, it decreases the excitability of the A-V junctional fibers between the atrial musculature and the A-V node, thereby slowing transmission of the cardiac impulse into the ventricles.
Weak to moderate vagal stimulation slows the rate of heart pumping, often to as little as one half normal. And strong stimulation of the vagi can stop completely the rhythmical excitation by the sinus node or block completely transmission of the cardiac impulse from the atria into the ventricles through the A-V mode. In either case, rhythmical excitatory signals are no longer transmitted into the ventricles. The ventricles stop beating for 5 to 20 seconds, but then some point in the Purkinje fibers, usually in the ventricular septal portion of the A-V bundle, develops a rhythm of its own and causes ventricular contraction at a rate of 15 to 40 beats per minute. This phenomenon is called ventricular escape.
Mechanism of the Vagal Effects. The acetylcholinereleased at the vagal nerve endings greatly increases the permeability of the fiber membranes to potassium ions, which allows rapid leakage of potassium out of the conductive fibers. This causes increased negativity inside the fibers, an effect calledhyperpolarization, which makes this excitable tissue much less excitable.
In the sinus node, the state of hyperpolarization decreases the “resting” membrane potential of the sinus nodal fibers to a level considerably more nega-tive than usual, to -65 to -75 millivolts rather than the normal level of -55 to -60 millivolts. Therefore, the initial rise of the sinus nodal membrane potential caused by inward sodium and calcium leakage requires much longer to reach the threshold potential for excitation. This greatly slows the rate of rhythmic-ity of these nodal fibers. If the vagal stimulation is strong enough, it is possible to stop entirely the rhyth-mical self-excitation of this node.
In the A-V node, a state of hyperpolarization caused by vagal stimulation makes it difficult for the small atrial fibers entering the node to generate enough elec-tricity to excite the nodal fibers. Therefore, the safetyfactor for transmission of the cardiac impulse throughthe transitional fibers into the A-V nodal fibers decreases. A moderate decrease simply delays con-duction of the impulse, but a large decrease blocks conduction entirely.
Effect of Sympathetic Stimulation on Cardiac Rhythm and Con-duction. Sympathetic stimulation causes essentially theopposite effects on the heart to those caused by vagal stimulation, as follows: First, it increases the rate of sinus nodal discharge. Second, it increases the rate of conduction as well as the level of excitability in all portions of the heart. Third, it increases greatly the force of contraction of all the cardiac musculature, both atrial and ventricular.
In short, sympathetic stimulation increases the overall activity of the heart. Maximal stimulation can almost triple the frequency of heartbeat and can increase the strength of heart contraction as much as twofold.
Mechanism of the Sympathetic Effect. Stimulation ofthe sympathetic nerves releases the hormone norepi-nephrine at the sympathetic nerve endings. The precisemechanism by which this hormone acts on cardiac muscle fibers is somewhat unclear, but the belief is that it increases the permeability of the fiber mem-brane to sodium and calcium ions. In the sinus node, an increase of sodium-calcium permeability causes a more positive resting potential and also causes increased rate of upward drift of the diastolic mem-brane potential toward the threshold level for self-excitation, thus accelerating self-excitation and, therefore, increasing the heart rate.
In the A-V node and A-V bundles, increased sodium-calcium permeability makes it easier for the action potential to excite each succeeding portion of the conducting fiber bundles, thereby decreasing the conduction time from the atria to the ventricles.
The increase in permeability to calcium ions is at least partially responsible for the increase in contrac-tile strength of the cardiac muscle under the influence of sympathetic stimulation, because calcium ions play a powerful role in exciting the contractile process of the myofibrils.
Related Topics