Chapter: Basic & Clinical Pharmacology : Vasodilators & the Treatment of Angina Pectoris
Clinical Pharmacology of Drugs Used to Treat Angina
CLINICAL PHARMACOLOGY OF DRUGS
USED TO TREAT ANGINA
Because
the most common cause of angina is atherosclerotic dis-ease of the coronaries
(CAD), therapy must address the underlying causes of CAD as well as the
immediate symptoms of angina. In addition to reducing the need for antianginal
therapy, such primary management has been shown to reduce major cardiac events
such as myocardial infarction.
First-line
therapy of CAD depends on modification of risk fac-tors such as smoking,
hypertension , hyperlipi-demia , obesity, and clinical depression. In addition,
antiplatelet drugs are very important.
Specific
pharmacologic therapy to prevent myocardial infarction and death consists of
antiplatelet agents (aspirin, ADP receptor blockers) and lipid-lowering agents,
especially statins. Aggressive therapy with statins has been shown to reduce
the incidence and severity of ischemia in patients during exercise testing and
the incidence of cardiac events (including infarc-tion and death) in clinical
trials. ACE inhibitors also reduce the risk of adverse cardiac events in patients
at high risk for CAD, although they have not been consistently shown to exert
antianginal effects. In patients with unstable angina and non-ST-segment
elevation myo-cardial infarction, aggressive therapy consisting of coronary
stenting, antilipid drugs, heparin, and antiplatelet agents is recommended. The
treatment of established angina and other manifestations of myocardial ischemia
includes the corrective measures previously described as well as treatment to
prevent or relieve symptoms. Treatment of symptoms is based on reduction of
myocardial oxy-gen demand and increase of coronary blood flow to the
potentially ischemic myocardium to restore the balance between myocardial
oxygen supply and demand.
Angina of Effort
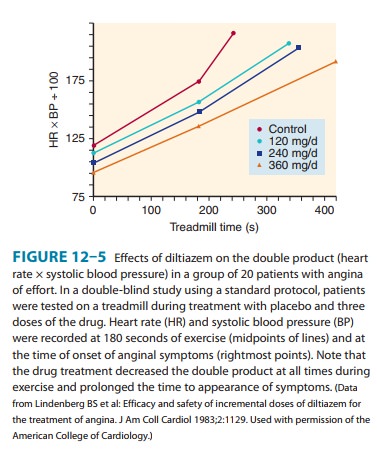
Many
studies have demonstrated that nitrates, calcium channel blockers, and β blockers increase
time to onset of angina and ST depression during treadmill tests in patients
with angina of effort (Figure 12–5). Although exercise tolerance increases,
there is usu-ally no change in the angina threshold, ie, the rate-pressure
prod-uct at which symptoms occur.
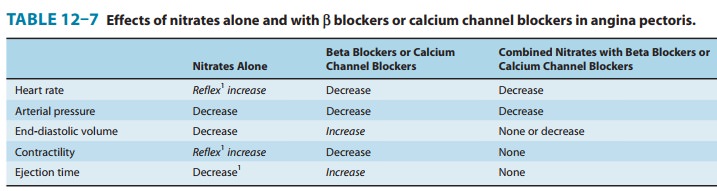
For
maintenance therapy of chronic stable angina, long-acting nitrates, calcium
channel-blocking agents, or β blockers may be chosen; the drug of choice
depends on the individual patient’s response. In hypertensive patients, monotherapy
with either slow-release or long-acting calcium channel blockers or β blockers may be
adequate. In normotensive patients, long-acting nitrates may be suitable. The
combination of a β
blocker with a calcium chan-nel blocker (eg, propranolol with nifedipine) or
two different calcium channel blockers (eg, nifedipine and verapamil) has been
shown to be more effective than individual drugs used alone. If response to a
single drug is inadequate, a drug from a different class should be added to
maximize the beneficial reduction of cardiac work while minimizing undesirable
effects (Table 12–7). Some patients may require therapy with all three drug
groups.
Surgical
revascularization (ie, coronary artery bypass grafting [CABG]) and
catheter-based revascularization (ie, percutaneous coronary intervention [PCI])
are the primary methods for promptly restoring coronary blood flow and
increasing oxygen supply in unstable or medically refractory angina.
Vasospastic Angina
Nitrates
and the calcium channel blockers are effective drugs for relieving and
preventing ischemic episodes in patients with variant angina. In approximately
70% of patients treated with nitrates plus calcium channel blockers, angina
attacks are completely abol-ished; in another 20%, marked reduction of
frequency of anginal episodes is observed. Prevention of coronary artery spasm
(with or without fixed atherosclerotic coronary artery lesions) is the
princi-pal mechanism for this beneficial response. All presently available
calcium channel blockers appear to be equally effective, and the choice of a
particular drug should depend on the patient. Surgical revascularization and
angioplasty are not indicated in patients with variant angina.
Unstable Angina & Acute Coronary Syndromes
In
patients with unstable angina with recurrent ischemic episodes at rest,
recurrent platelet-rich nonocclusive thrombus formation is the principal
mechanism. Aggressive antiplatelet therapy with a combination of aspirin and
clopidogrel is indicated. Intravenous heparin or subcutaneous
low-molecular-weight heparin is also indicated in most patients. If
percutaneous coronary intervention with stenting is required, glycoprotein IIb/IIIa
inhibitors such as abciximab should be added. In addition, therapy with
nitroglyc-erin and β
blockers should be considered; calcium channel block-ers should be added in
refractory cases for relief of myocardialischemia. Primary lipid-lowering and ACE-inhibitor
therapy should also be initiated.
Related Topics