Chapter: Clinical Anesthesiology: Clinical Pharmacology: Cholinesterase Inhibitors & Other Pharmacologic Antagonists to Neuromuscular Blocking Agents
Cholinergic Pharmacology: Clinical Pharmacology
CLINICAL PHARMACOLOGY
General Pharmacological Characteristics
The increase in acetylcholine caused by
cholinester-ase inhibitors affects more than the nicotinic recep-tors of
skeletal muscle (Table 12–2). Cholinesterase
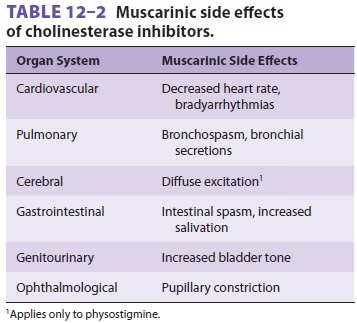
inhibitors can act at cholinergic
receptors of several other organ systems, including the cardiovascular and
gastrointestinal systems.
Cardiovascular
receptors—The
predominantmuscarinic effect on the heart is bradycardia that can progress to
sinus arrest.
Pulmonary
receptors—Muscarinic
stimulationcan result in bronchospasm (smooth muscle contraction) and increased
respiratory tract secretions.
Cerebral
receptors—Physostigmine
is acholinesterase inhibitor that crosses the blood– brain barrier and can
cause diffuse activation of the electroencephalogram by stimulating muscarinic
and nicotinic receptors within the central nervous system. Inactivation of
nicotinic acetylcholine receptors in the central nervous system may play a role
in the action of general anesthetics. Unlike physostigmine, cholinesterase
inhibitors used to reverse neuromuscular blockers do not cross the blood–brain
barrier.
Gastrointestinal
receptors—Muscarinicstimulation
increases peristaltic activity (esophageal, gastric, and intestinal) and
glandular secretions (eg, salivary). Postoperative nausea, vomiting, and fecal
incontinence have been attributed to the use of cholinesterase inhibitors.
Unwanted muscarinic side effects are
mini-mized by prior or concomitant administration of anticholinergic
medications, such as atropine sulfate or glycopyrrolate. The duration of action
is similar among the cholinesterase inhibitors. Clearance is due to both
hepatic metabolism (25% to 50%) and renal excretion (50% to 75%). Thus, any
pro-longation of action of a nondepolarizing muscle relaxant from renal or
hepatic insufficiency will probably be accompanied by a corresponding increase
in the duration of action of a cholinesterase inhibitor.
As a rule, no amount of cholinesterase
inhibitor can immediately reverse a block that is so intense that there is no
response to tetanic peripheral nerve stimulation. Moreover, the absence of any
palpable single twitches following 5 sec of tetanic stimulation at 50 Hz implies
a very intensive blockade that can-not be reversed. Excessive doses of
cholinesterase inhibitors may actually prolong recovery. Some evi-dence of
spontaneous recovery (ie, the first twitch of the train-of-four [TOF]) should
be present before reversal is attempted. The posttetanic count (the number of
palpable twitches after tetanus) generally correlates with the time of return
of the first twitch of the TOF and therefore the ability to reverse intense
paralysis. For intermediate-acting agents, such as atracurium and vecuronium, a
palpable posttetanic twitch appears about 10 min before spontaneous recovery of
the first twitch of the TOF. In contrast, for longer-acting agents, such as
pan-curonium, the first twitch of the TOF appears about 40 min after a
palpable posttetanic twitch.The time required to fully reverse a
nondepo-larizing block depends on several factors, including the choice and
dose of cholinesterase inhibitor administered, the muscle relaxant being
antagonized, and the extent of the blockade before reversal. For example,
reversal with edrophonium is usually faster than with neostigmine; large doses
of neostigmine lead to faster reversal than small doses; intermediate-acting
relaxants reverse sooner than long-acting relaxants; and a shallow block is
easier to reverse than a deep block (ie, twitch height >10%). Intermediate-acting muscle relaxantstherefore
require a lower dose of reversal agent (for the same degree of blockade) than
long-acting agents, and concurrent excretion or metabolism provides a
proportionally faster reversal of the short- and intermediate-acting agents.
These advantages can be lost in conditions associated with severe end-organ
disease (eg, the use of vecuronium in a patient with liver failure) or enzyme
deficien-cies (eg, mivacurium in a patient with homozygous atypical
pseudocholinesterase). Depending on the dose of muscle relaxant that has been
given, sponta-neous recovery to a level adequate for pharmaco-logical reversal
may take more than 1 hr with long-acting muscle relaxants because of their
insig-nificant metabolism and slow excretion. Factors associated with faster
reversal are also associated with a lower incidence of residual paralysis in
the recovery room and a lower risk of postoperative respiratory complications.
A reversal agent should be routinely
given to patients who have received nondepolarizingmuscle relaxants unless full
reversal can be demon-strated or the postoperative plan includes continued
intubation and ventilation. In the latter situation, adequate sedation must
also be provided.
A peripheral nerve stimulator should
also be used to monitor the progress and confirm the ade-quacy of reversal. In
general, the higher the fre-quency of stimulation, the greater the sensitivity
ofthe test (100-Hz tetany > 50-Hz tetany or
TOF > single-twitch height). Clinical signs
of adequate reversal also vary in sensitivity (sustained head lift > inspiratory force > vital capacity > tidal volume). Therefore, the suggested end points
of recov-ery are sustained tetanus for 5 sec in responseto a 100-Hz stimulus in
anesthetized patients or sus-tained head or leg lift in awake patients. Newer
quantitative methods for assessing recovery from neuromuscular blockade, such
as acceleromyogra-phy, may further reduce the incidence of residual
postoperative neuromuscular paralysis.
Related Topics