Chapter: Case Study in Obstetrics and Gynaecology: Emergency Gynaecology
Case Study Reports: Pelvic Pain
PELVIC PAIN
History
A
27-year-old woman complains of left iliac
fossa pain. The pain started
while she was asleep the night before
last and she
says it woke
her suddenly. Initially the pain was
con- stant and severe
and she was
unable to get
out of bed
for a few hours. She
felt nauseated and did
not eat anything all day yesterday. There was no associated bleeding or discharge and there
are no bowel
or urinary symptoms. Today the pain
is still present
but much improved and she has been able to have breakfast.
She has had similar episodes twice in the past but they were not as severe
or long-lasting. She had never been pregnant and uses the progesterone only pill (POP) for contraception. She has been with her partner for 3 years and has not had any previous sexually transmitted
infections. There is no other medical history of note.
Examination
The
temperature is 37.1°C,
heart rate 76/min
and blood pressure
122/70 mmHg. The abdomen is slightly distended and tender in the suprapubic and left iliac
fossa regions with some rebound tenderness but no guarding.
No masses are palpable. Speculum
exam- ination is normal
and she is tender in the left adnexa on bimanual examination, but no cervical
excitation or masses are evident.
Questions
·
What is the differential diagnosis?
·
How would you manage this patient?
Answer:
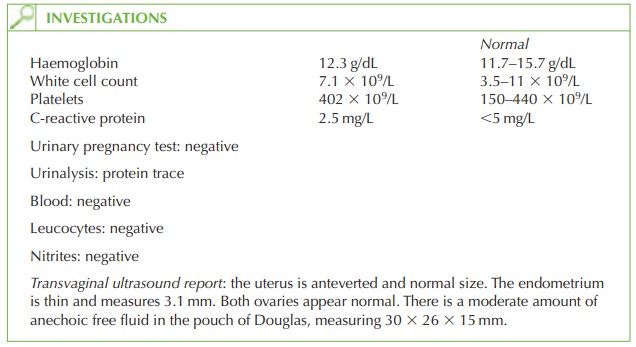
The
sudden onset of left iliac
pain suggests rupture,
haemorrhage or torsion
of an ovarian cyst. In cases
of torsion of the ovary
this would normally
result in vomiting
and systemic upset, whereas
this woman’s condition has in fact
improved. In addition, an adnexal mass would be visible on ultrasound. Haemorrhage into a cyst would be seen on transvaginal
ultrasound scan as an echogenic ovarian enlargement.
If
a cyst ruptures then it is common
for the ovary
to appear ultrasonographically normal afterwards but the finding
of free fluid in the pouch of Douglas suggests
the former pathology.
Thus the diagnosis is likely to be a ruptured ovarian
cyst. Alternative diagnoses may include irritable bowel
syndrome or possibly renal colic, though
urinalysis does not
show haematuria.
Management
The
patient is already
improving and the
free fluid which
is causing the
peritoneal irrita- tion (and
the rebound tenderness) is expected to resolve spontaneously. Therefore imme-
diate management is supportive with analgesia.
In
the longer term,
the woman should
be advised to use a different contraceptive as the POP is known to be associated with an increased incidence of ovarian
cysts and it seems
from the history that this is the third episode
for this woman.
Related Topics