Chapter: Case Study in Obstetrics and Gynaecology: Emergency Gynaecology
Case Study Reports: Bleeding In Pregnancy
BLEEDING IN PREGNANCY
History
A
19-year-old woman presents at 13 weeksŌĆÖ
gestation with vaginal
bleeding and a smelly
watery discharge. She feels generally unwell and has had fevers
for the last 48 h. She ini- tially thought she had gastroenteritis as she had reduced appetite, abdominal pain, vomi- ted and had loose stools.
All
her booking bloods
were normal and the 11 week ŌĆśnuchalŌĆÖ scan was reassuring. She had a previous
normal vaginal delivery
at 38 weeksŌĆÖ gestation. She has no significant
gynaecological or general
medical history.
Examination
On
examination the temperature is 38.1┬░C,
pulse 96/min and blood pressure
110/68 mmHg. She looks flushed and her peripheries are warm. Chest and cardiac examin-ation are normal.
She is tender over the uterus, which feels approximately 14 weeksŌĆÖ size. There is no guarding or rebound. On speculum
examination the cervical os is closed but an offensive
blood-stained discharge is seen. Bimanual
examination reveals a very tender
and hot uterus that also feels
ŌĆśboggyŌĆÖ. No adnexal
masses are palpable but bilateral adnexal tenderness is evident.
Questions
┬Ę
What is the diagnosis?
┬Ę
Why is this presentation rela-
tively uncommon in current clin- ical practice?
┬Ę
How
would you further
investi- gate and manage
this woman?
ANSWER
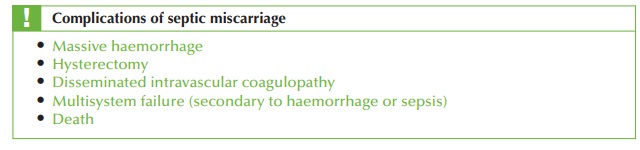
The
woman is pregnant with a dead
fetus and signs
of sepsis. This
is referred to as a sep-
tic miscarriage. This used to be a common diagnosis
due to the high incidence
of illegal terminations
performed by unqualified people without appropriate sterile technique,
instruments or anaesthesia. Since the 1967 Abortion Act, morbidity and mortality from septic miscarriage has fallen
dramatically but it remains a cause of maternal mortality, often because it is not
recognized early enough. It should therefore be recognized promptly and treated aggressively.
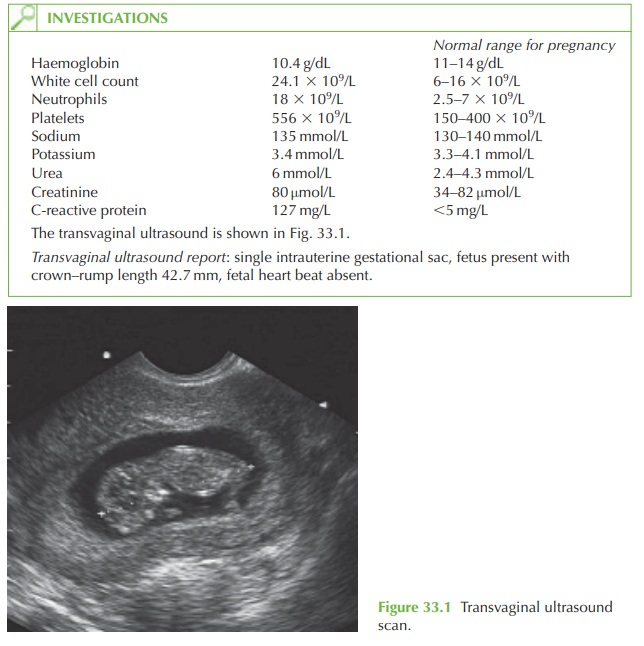
Further investigations necessary
are: blood cultures; liver function tests; coagulation screen, group and save;
high vaginal and endocervical swabs.
Management
┬Ę
The woman should be admitted and
commenced on broad-spectrum intravenous antibiotics pending culture and sensitivity.
┬Ę
Aggressive intravenous fluids should
be given as she has
intravascular depletion due
to sepsis (vasodilatation) and vomiting.
┬Ę
Evacuation of retained products of conception should
be arranged urgently, once the first
dose of antibiotics has been given.
┬Ę
A
senior gynaecologist should
be involved as the risks
of uterine perforation or of mas- sive haemorrhage are significant in the presence
of sepsis.
┬Ę
A
urinary catheter should
be inserted to monitor renal
function.
┬Ę
The
woman may need transfer to the intensive care unit depending on her cardiovas- cular, respiratory and
haematological state.
Related Topics