Chapter: Modern Medical Toxicology: Cardiovascular Poisons: Diurets, Antihypertensives and Antiarrhythmics
Beta Adrenergic Antagonists (Beta Blockers) - Sympatholytic Drug Cardiovascular Poison
Beta Adrenergic Antagonists (Beta Blockers)
Beta-adrenergic
blocking agents compete with endogenous and/or exogenous beta-adrenergic
agonists for receptor sites. Depending upon the agent and its relative
selectivity for beta1 (located primarily in the heart) and beta2 receptors
(located chiefly in bronchial smooth muscle and blood vessels), principal
pharmacologic effects include a lowering of blood pressure, negative inotropic
and chronotropic effects, and depressed AV conduction.
Examples
Acebutolol,
adimolol, alprenolol, amosulalol, arotinolol, atenolol, befunolol, betaxolol,
bevantolol, bisoprolol, bopindolol, bucindolol, bufetolol, bufuralol,
bunitrolol, bupran-olol, butofilolol, carazolol, carteolol, carvediolol,
celiprolol, cetamolol, coloranolol, cycloprolol, dilevalol, divelalol,
draquinolol, esmolol, espanolol, flestolol, indenolol, labetalol, landiolol,
levobetaxolol, levobunolol, levomoprolol, medrox-alol, mepindolol, metipranolol,
metoprolol, nadolol, nebivolol, nifenalol, nipradilol, oxprenolol, penbutolol,
pindolol, prac-tolol, propranolol, sotalol, teratolol, tilisolol, and timolol.
First
generation beta blockers (nadolol, propranolol, pind-olol, labetalol, sotalol,
timolol, etc.) are antagonists at both beta1 and beta2 adrenoceptors and are
known to aggravate asthma, obstructive airway disease, peripheral artery
disease, and diabetes mellitus. Second generation drugs such as acebutolol,
atenolol, and metoprolol are selective for beta1 adrenoceptors, and therefore
relatively safer. Recently, a new beta-adrenergic receptor referred to as beta3
adrenoceptor has been discovered. Classic beta blockers are all agonists (not
antagonists) at this receptor.*
Uses
Beta-blockers
are used in the treatment of hypertension, angina, arrhythmias, cardiomyopathy,
migraine headaches, and thyro-toxicosis. Ophthalmic products are used in the
treatment of glaucoma.
Adverse Effects
· Bradycardia, dizziness, fatigue,
diarrhoea, sleepiness, confusion, depression, and headache. While CNS effects
at therapeutic doses are more often associated with more lipid soluble agents
(propranolol, metoprolol), in overdose all agents may cause significant CNS
depression. Effects range from drowsiness and lethargy to obtundation and coma.
Therapeutic doses of beta adrenergic blocking agents may cause bronchospasm in
susceptible patients. Worsening angina may develop in patients after withdrawal
from chronic beta blocker therapy.
· Drug-induced retroperitoneal
fibrosis has been reported following treatment with practolol, atenolol, and
oxpre-nolol.
·
Propranolol can cause hypoglycaemia and resultant seizures
in diabetics treated with oral hypoglycaemics or insulin and in non-diabetics
who are dieting, fasting and exercising. The clinical effects of hypoglycaemia
(tachy-cardia and sweating) may be absent due to beta-blockade in such cases.
·
Propranolol appears to cross the placenta and may result in
intrauterine growth retardation, bradycardia, hypogly-caemia, respiratory depression
and impaired response to anoxic stress. Acebutolol, atenolol, betaxolol,
labetalol, metoprolol, nadolol, propranolol and timolol are excreted in human
breast milk.
Drug Interactions
·
Severe bradycardia, conduction
blocks and hypotension have been reported in patients taking calcium
antagonists and beta blockers at therapeutic doses.
·
Complete atrioventricular block,
bradycardia, hypotension and biventricular failure have been reported after
thera- peutic use of digoxin and propranolol.
·
Quinidine inhibits metabolism of
timolol and increases the degree of beta blockade experienced after use of
timolol eye drops.
·
Dystonia may develop if propranolol
and gabapentin are given together, due to synergistic effect.
Clinical (Toxic) Features
· Lipid soluble beta blockers such as
propranolol, oxprenolol, labetalol, metoprolol, pindolol, and timolol are
capable of producing serious toxicity. Fatalities have been reported with
propranolol, metoprolol, acebutolol, and oxprenolol. Co-ingestion of alcohol is
nearly always catastrophic. Labetalol and atenolol are said to be safest in
overdose and rarely cause death.
· Manifestations of overdose include
hypotension, brady-cardia, arrhythmias, delirium, seizures, mydriasis, coma,
and respiratory failure. Hypoglycaemia is common in chil-dren. Bradycardia and
hypotension are the most common effects in beta blocker overdose. Complications
of profound hypotension may include acute renal failure, respiratory failure
and non-cardiogenic pulmonary oedema.
· Other cardiovascular effects may
include atrioventricular blocks, intraventricular conduction delays,
ventricular arrhythmias, pulmonary oedema and cardiac arrest. An irregular
pulse may be a sign of conduction defects or arrhythmias. Asystole has also
been reported.
· Pindolol has greater beta-agonist
properties and overdoses have been associated with hypertension and
tachycardia.
· CNS depression is common in patients
with significant cardiovascular toxicity. Seizures have been frequently
reported with propranolol overdose. Sotalol is notorious for causing delayed
toxicity, and for inducing a prolonged QT interval and ventricular arrhythmias.
Fatalities are common.
· Metabolic acidosis may develop in
patients with profound hypotension or seizures.
· Ophthalmic preparations containing
beta-blockers may cause systemic manifestations. Increased airway resistance
(usually in asthmatics), hypoglycaemia, fatigue, behav-ioural abnormalities,
and diplopia may be noted.
·
Abrupt stoppage of beta blockers after chronic use may
result in rebound hypertension, tachycardia, palpitations, tremor, headache,
and sweating. Patients with angina may develop myocardial infarction.
Diagnosis
Plasma
levels of these agents are not clinically useful and are not routinely
available.
Treatment
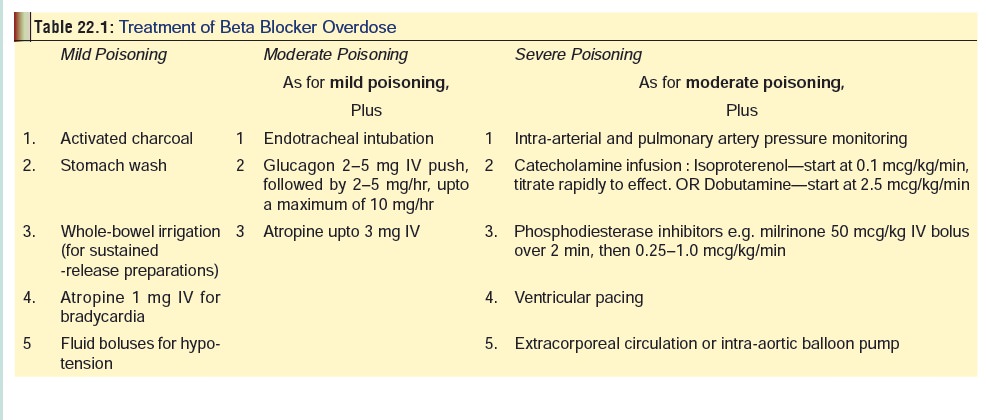
• Outlined in Table 22.1.
• Glucagon is said to have antidotal action.
It produces a positive chronotropic and inotropic cardiac effect, which occurs
despite beta-blockage. The drug has been reported to increase myocardial
contractility in patients refractive to isoproterenol. Glucagon is thought to
activate the adenylate cyclase system at a different site than isoproterenol.
If the patient responds at a particular dose of glucagon, start an hourly
infusion at the response dose (e.g. if a patient responds to 10 mg, then start
an infusion at 10 mg per hour).
• Monitor electrolytes and renal function in
patients with hypotension.
• Monitor blood glucose in symptomatic
children and diabetics.
• Institute continuous cardiac monitoring,
monitor blood pressure, and obtain an ECG.
• Obtain a chest X-ray in patients with
respiratory depression, significant hypotension or evidence of pulmonary
oedema.
• Patients, who at presentation show
evidence of significant cardiovascular (bradycardia, heart failure, heart
block, hypotension, electromechanical dissociation, asystole, new bundle branch
block or widened QRS complex) respiratory (respiratory depression,
bronchospasm, or pulmonary oedema) or neurologic toxicity (CNS depres- sion or
seizures), independent of the dose ingested, should be admitted to a monitored
setting for at least 24 hours of observation and treatment.
• Hypotension usually responds to
intravenous glucagon, atropine, isoproterenol or pacing. Atropine reduces vagal
stimulation and subsequently increases heart rate. Isoproterenol is a beta
agonist which competitively antagonises the effect of the beta-blocker. It is
used for temporary control of haemodynamically signifi-cant bradycardia;
generally other modalities (atropine, dobutamine, pacing) should be used first
because of the tendency to develop ischaemia and arrhythmias with
isoproterenol. 1 mg of isoproterenol is added to 250 ml of dextrose 5% in
water, for a final concentration of 4 mcg/ml. Infuse 2 mcg/min, gradually
titrating to 10 mcg/min as needed, to desired response. If hypotension
persists, administer dopamine or noradrenaline. Refrac-tory cardiotoxicity may
respond to calcium chloride. Intra-aortic balloon pump has been used
successfully after pharmacologic therapy failed, in cases of severe propranolol
and atenolol poisoning.
• Extracorporeal membrane oxygenation may be
useful in providing haemodynamic support for arrhythmias, hypotension, and
heart failure unresponsive to glucagon, dopamine, noradrenaline, adrenaline, or
pacemaker.
• Hypoglycaemia should be managed with intravenous
dextrose. Bronchospasm responds to salbutamol (0.25 to 0.5 ml in 2 to 4.5 ml of
normal saline delivered every 4 to 6 hours per nebuliser).
• Nadolol, sotalol, acebutolol, and atenolol
are haemodi-alysable. Propranolol, metoprolol, and timolol are not removed by
haemodialysis. Haemoperfusion is said to be effective in nadolol, atenolol, and
sotalol overdose. However, it should be considered only when treatment with
glucagon and other pharmacotherapy fails.
Related Topics