Chapter: Essentials of Psychiatry: Hypnosis
Applications of Hypnosis
Applications
of Hypnosis
General Considerations
Because
of the intrinsic qualities of the hypnotic state, it can be an effective
adjunct to the treatment of a variety of symptoms and problems, both in
psychiatry and in medicine in general. The first criterion to consider is the
patient’s level of hypnotizability. Once it has been determined that the
patient has usable hypnotic capacity (defined by high scores in hypnotizability
scales), a dis-cussion about the nature of the hypnotic process follows. It is
important at this point to dispel any myths and correct miscon-ceptions the
patient may have about the process. This includes the cooperative nature of the
hypnotic process, rather than the “tell me what to do” most patients expect.
Finally, the therapist must decide whether the problem presented by the patient
is ame-nable to hypnotic intervention or whether other steps should be taken
instead.
We have
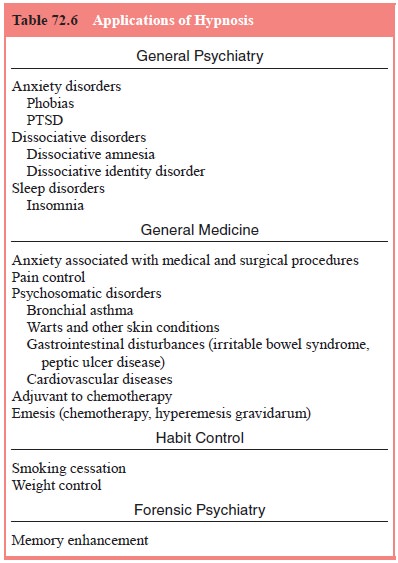
divided the discussion of the applications of hypnosis into five areas: general
psychiatry, general medicine, psychosomatic disorders, habit control and
forensic psychiatry (Table 72.6).
Application in Psychiatric Disorders
The use
of hypnosis in the context of conventional psycho-therapy can facilitate the therapeutic
process in a number of ways. For example, hypnotherapeutic techniques may be
used to enhance the patient’s sense of self, restructure traumatic and phobic
experiences, or access to repressed memories that havenot emerged with use of
other techniques. This is true not only of painfully repressed memories but
also of situations in which both the patient and the therapist have worked on
resistance issues and feel that some additional leverage is necessary. In
conventional psychotherapy, the transference is observed and analyzed; in
hypnosis, the transference is used as part of the therapeutic process.
Conventional
psychoanalytic psychotherapy involves observation and analysis of the meaning
of the transference reaction that arises during therapeutic interactions. On
the other hand, when hypnosis is used, transference is not avoided or bypassed
but may be amplified. All the usual therapeutic rules and processes of
psychotherapy apply when hypnosis is used in the psychotherapy context, which
may intensify or accelerate the therapeutic process.
Because
of the intense emotions that are characteristic of the hypnotic retrieval
(which facilitates expression of inner fantasies), intense feelings and deep
personal experiences may be elicited. Some patients may find that the hypnotic
state facilitates a sense of infantile dependency in which the therapist
becomes the transferential object. The quality of this transference reaction
will be based on the patient’s early object relations, just as in any other therapeutic
relationship. Indeed, the transference reaction may develop so fast that the
inexperienced therapist may not have the opportunity to recognize it or may do
so too late. The difference here is the intensity of the feelings developed as
a result of the strong emotions that arise during trance. As in the case of
victims of abuse, the therapist may use the transference relationship under
hypnosis to foster the patient’s ability to help herself or himself.
The
difficult aspect of doing hypnosis is not the induction of the hypnosis trance,
but what happens once the patient is under trance. Remember that all hypnosis
is self-hypnosis. Thus, there are two factors which will predict the success of
the hypnosis in-tervention: the patients’ hypnotizability and the therapeutic
skills of the therapist.
Anxiety Disorders
Anxiety
disorders are among the most widely prevalent psy-chiatric disturbances. They
afflict as much as 15% of the pop-ulation (Myers et al., 1984). Anxiety can be seen as a state of hyperarousal
experienced by both emotional and somatic discomfort. Patients describe their
experience in physical terms, such as palpitations, gastrointestinal
discomfort, chest pain, sweating and motor restlessness. Among anxiety
disor-ders most responsive to hypnotic intervention are generalized anxiety
disorder, panic disorder, phobias and post traumatic anxiety disorders.
Most of
the strategies in the treatment of anxiety disor-ders employing hypnosis
combine instructed physical relaxation with a restructuring of cognition, using
imagery coupled with physical relaxation. As in the treatment of anxiety
disorders by systematic desensitization (Marks et al., 1968) or progressive relaxation, patients are instructed to
maintain a physical sense of relaxation (e.g., floating) while picturing the
feared situation or stimulus. It is important that the relaxation instruction
use an image that connotes reduced somatic tension, such as floating or
lightness, rather than being a direct instruction to relax. The more cognitive
term “relax” may actually induce more anxiety, whereas affiliation with a
somatic metaphor usually produces some reduction in tension. Unlike systematic
desensitization, hypnosis produces a physically relaxed state that can be
rapidly achieved with a quick induction. Also different from systematic
desensitization, the coupling of relaxation to a fearful stimu-lus does not
require the development or working through of a hierarchy.
A typical
self-hypnosis induction can be rapid. For exam-ple, a patient can be told:
Now just
get as comfortable as you can. There are many ways to enter a state of
self-hypnosis. One simple but useful method is to count to yourself from 1 to
3. On 1, do one thing: look up. On 2, do two things: slowly close your eyes and
take a deep breath. On 3, do three things: let your eyes relax but keep them
closed, let your breath out, and let your body float. Then let one hand or the
other float up into the air like a buoyant balloon. This is your signal to
yourself and to me that you are ready to concentrate.
Initially,
the use of hypnosis in the session can help in demon-strating to patients that
they have a greater degree of control over somatic responsiveness than they had
imagined. It is often useful to begin by teaching patients to create a place in
their mind’s eye where they feel safe and secure. On occasion, it helps the
subjects to learn how to project their image onto an imaginary screen. Later,
they can learn to manipulate the screen by making it either bigger or smaller,
having the screen nearer or farther away, as needed:
Just
allow your body to float, as if you were floating in a bath, a lake, or a hot
tub. Enjoy this sense of floating lightness. Now, picture in your mind’s eye an
imaginary screen. It might be a movie screen, a television screen, or a piece
of clear blue sky. First picture a pleasant scene, somewhere you enjoy being.
Allow the
patient to experience this state for a minute or two, then inquire about the
experience:
With your
eyes closed and remaining in this state of concentra-tion, describe how your
body is feeling right now. What image are you picturing?
After
receiving the answers, add:
Notice
how you can use your store of memories and fantasies to help yourself and your
body feel better.
After
they have learned to manipulate the screen and their physical sensations,
patients may be ready to do therapy work. They may, for example, learn to
re-create the physical state of relaxation while projecting the fearful
situation onto the screen. This, then, becomes a useful procedure by which to
control and obtain mastery over anxiety-producing situations by dissoci-ating
the somatic reaction from the psychological response to the feared stimulus.
Initially, the patient is asked to re-create the physical feeling of
relaxation. Then, the patient projects onto the screen images associated with
the feared situation, only this time the somatic reactions associated with
anxiety do not develop. On occasion, it helps for patients to foresee likely
physical sensations or situations associated with a fearful expe-rience to
master them. For example, in the case of plane phobia, the patient can learn to
couple the real sensation of floating in the air with the hypnotic experience:
“Learn to float with the plane”.
Patients
may also use the trance state as a means of facing their concerns more
directly. As in the preceding cases, they may make use of the screen technique.
They can achieve this by plac-ing an image of an upcoming performance or
fearful situation on one side of the screen, testing out various strategies for
mastering the situation on the other side.
Other
approaches using hypnosis have included instructing patients in a trance to
imagine that they are literally somewhere else, away from the fearful stimulus,
thus separating themselves from the anxiety-producing experience (Erickson and
Haley, 1967). Positive reinforcement or “ego-strengthening” techniques have
also been used; for example, hypnotic instructions are given to patients
suggesting that their capacity to master the situation and their response to it
will improve (Crasilneck and Hall, 1985). There is little reason to use
uncovering techniques seeking to link anxiety to some early traumatic
experience in cases of phobia or generalized anxiety disorders. This is
different in cases of PTSD (DSM-IV-TR), however, in which more work may be
needed to confront and place into context the traumatic experience.
Certainly,
in some cases, understanding the cause of the feared situation may help resolve
the conflict. One of the tech-niques used to facilitate the recovery of
traumatic memories associated with fearful situations is the affect bridge
technique (Watkins, 1987).
Post Traumatic Stress Disorder
Trauma constitutes
a sudden discontinuity in both physical and mental experiences. The effect of
the traumatic experience forces the victim to reorganize mental and
psychophysiological proc-esses to buffer the immediate impact of the trauma.
This process is meant to be an adaptive mechanism to maintain psychologi-cal
control during a time of enormous stress. Unfortunately, a number of trauma
victims go on to suffer acute or chronic symp-toms, such as dissociation,
intrusive thoughts, anxiety, with-drawal and hyperarousal, leading to a
diagnosis of acute stress disorder or PTSD.
There may
be a relationship during childhood between stress, such as early trauma, and
high hypnotizability. In support of this idea are reports of high
hypnotizability in children who were victims of severe punishment during
childhood (Nash and Lynn, 1986; Spiegel and Cardeña, 1991). It is possible that
the impact of the stress suffered encouraged them to use their self-hypnotic
abilities more effectively (Kluft, 1984, 1992; Spiegel et al., 1982).
The major
categories of symptoms in PTSD are similar to the components of the hypnotic
process (American Psychiatric Association, 1994; Maldonado and Spiegel, 2002a).
Hypnotic absorption is similar to the intrusive reliving of traumatic events
experienced by these patients. When in a flashback, trauma victims become so
absorbed in the memories of the traumatic event, they lose touch with their
present surroundings and even forget that the events took place in the past.
Likewise, highly hypnotizable individuals may become so intensely absorbed in
the trance experience that they can reenact a previous life event (during
hypnotic age regression) as if they were reliving it. A hypnotized patient may
dissociate a body part to the extent of not recognizing it as part of his or
her body. Similarly, PTSD patients may dissociate feelings to the extent of
experiencing the so-called psychic numbing. This allows them to disconnect
current affects from their everyday experience in an attempt to avoid emotions
triggering memories associated with the trauma. Finally, suggestibility is
comparable to hyperarousal. The heightened sensitivity to environmental cues
observed in those patients suffering from PTSD is similar to that experienced
by a hypnotized individual who responds to suggestions of coldness by
shivering.
Because
many patients suffering from PTSD are highly hypnotizable, and because of the
resemblance between the symp-toms of PTSD and the hypnotic phenomena, it makes
sense to use hypnosis in its treatment. If patients suffering from PTSD are
unknowingly using their own hypnotic capacities (Kluft, 1991, 1992; Maldonado
and Spiegel, 2002a; Spiegel 1986, 1989; Spiegel et al., 1988), it is therapeutically useful to teach them how to
enter, access and control their trance potential. Hypnosis may be invaluable as
a tool to access previously dissociated traumatic material.
We do not
refer here to uncontrolled abreaction. The purpose is not simply to help the
patient remember the trauma, because in a way, every time a patient goes
through a flashback, an uncontrolled abreaction is experienced. An abreaction
that is not conducted within the context of cognitive restructuring and before
new defenses are in place can lead to the further retraumatization of the patient
(Kluft, 1992; Spiegel, 1981). At the end of the following section (Dissociative
Disorders), we summarize a comprehensive approach to the use of hypnosis in the
treatment of psychiatric syndromes associated with severe trauma.
Dissociative Disorders
Hypnosis
is one of the most helpful tools in the treatment of patients suffering from
dissociative disorders (Maldonado and Spiegel, 2002a; Maldonado et al., 2000). As a rule, these patients
experience their symptoms (i.e., fugue states, dissociated identities and
blackouts) as occurring unexpectedly and beyond their control. Because these
patients are unknowingly using their hypnotic capacities, it makes sense to
teach them how to turn their weakness into a strength (Maldonado and Spiegel,
1995). Hypnosis can be used formally both as a diagnostic tool and for
therapeutic purposes. The hypnotic state can be seen as a controlled form of
dissociation (Nemiah, 1985). Hypnosis is useful in the treatment of these
patients, first in determining whether they have a dissociative disorder, and
second in providing rapid access to these dissociated states. When used by the
therapist in the context of treatment, it can demonstrate to patients the
amount of control they have over this state, which they normally experience as “automatic
and unpredictable”. This not only serves to teach patients how to control
dissociation but also allows them to establish a process of communication that
will eventually lead to a reduction in spontaneous dissociative symptoms.
Therapists must remember that many of these patients have suffered physical,
emotional, or sexual abuse. It is imperative that we recognize and take account
of the impact of whatever trauma occurred and help patients work through their
reactions to it, as in the case of PTSD. Recognizing and teaching patients with
dissociative disorders how to master their capacity to dissociate are among the
most important psychotherapeutic tasks in the course of their treatment
(Maldonado and Spiegel, 2002a; Maldonado et
al., 2000).
We can
make use of hypnotic techniques as a way to help patients access repressed and
dissociated memories. Teaching patients to use self-hypnosis allows them to
obtain a sense of control over their symptoms and eventually their lives. The
repression or dissociation of traumatic events and the realities that surround
them may serve a defensive pur-pose of avoiding painful affect associated with
the memories. The memories are there, either transformed or interspersed with
fantasy. Our approach to the treatment of these victims is directed at helping
them acknowledge the extent of the emo-tional pain caused by the trauma. Then,
through therapy, we can assist in the development of mature and adequate coping
mechanisms that will allow the patient to place the experi-ence into proper
perspective. The goal is to allow the patient to come to terms with the trauma
and to redefine herself or himself in view of the past, but with a firm hold on
the reali-ties of the present.
Dissociation
as a defense serves a dual purpose. It rep-resents an effort to preserve some
form of control, safety and identity when faced with overwhelming stress. At
the same time, victims use it in an attempt to separate themselves from the
full impact of the trauma. Unfortunately, these individuals may ward off
memories of the trauma so well that they may act as if it is not happening and
later as if it never happened. Some individuals can so effectively repress
traumatic memories that they become unable consciously to work through them. As
a consequence, they are unable to put the facts surrounding the events
associated with the trauma into perspective, but slowly, the dissociated
feel-ings and memories leak into consciousness. This creates some of the
classic symptoms associated with PTSD and DID, such as flashbacks or intrusive
thoughts.
The
advantage of using hypnosis comes from the facilita-tion of the recovery of
affect or memories, the ability to dis-sociate memories from cognition, and the
speed with which the process is achieved. Finally, because of the relationship
between a history of childhood abuse and trance, these patients are usually
highly hypnotizable (Chu and Dill, 1990; Hilgard, 1984; Nash and Lynn, 1986;
Putman, 1993; Spiegel, 1988, 1990; Spiegel et
al., 1988).
Many
former victims of childhood abuse may unknow-ingly use their hypnotic
capacities to keep out of awareness the content of traumatic memories and in
effect create different de-grees of psychiatric illness (Sanders and Giola,
1991; Spiegel, 1984, 1986, 1989; Spiegel et
al., 1988; Terr, 1991). Teaching these patients self-hypnosis is a way of
turning a weakness into a strong tool for self-mastery and control. The
controlled use of hypnosis, then, becomes a way systematically to access
previously dissoci-ated material.
The Condensed Hypnotic Approach
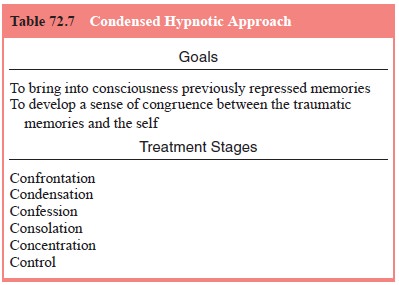
The use
of hypnosis in the treatment of PTSD and disso-ciative disorders can be
conceptualized as having two major goals, which can be achieved by the use of
six different tech-niques (Maldonado and Spiegel, 1994, 1995, 2002b; Spiegel,
1992) (Table 72.7). The goals are to bring into consciousness previously repressed memories and to develop a sense
of congruence between memories
associated with the traumatic experience
and current self-images. By making conscious pre-viously repressed memories,
the patient has the opportunity to understand, accept and restructure them.
These goals are achieved by working through six treatment stages:
confronta-tion, condensation, confession, consolation, concentration and
control.
First the
patient must confront the trauma.
The therapist helps the patient recognize and understand the factors involved
in the development of the symptoms for which help is now being
sought.
Hypnosis is then used to help the patient condense
the traumatic memories. The hypnotic experience can be used to define a
particularly frightening memory during the revision of the patient’s history,
which summarizes or condenses the main conflicts. The focused concentration
achieved during the hypnotic state not only can facilitates recall of traumatic
material but also helps place boundaries around it. After memories are
recovered, we can help patients restructure them and even “become aware of
things you did at the moment of trauma to survive”. Once memories are
recovered, patients usually need to confess
feelings and experiences of which they are profoundly ashamed. These are usually things that they may have told no one
else before; in fact, they have been running from them all their lives. At this
time, the therapist must convey a sense of “being present” for the patient
while remaining as neutral as possible. This is followed by the stage of consolation. Here, the therapist needs
to be emotionally available to the patient. This stage must be carried on with
caution and in a most professional manner. Therapists should be aware that the
body and emotional boundaries of these patients may have been violated in the
past. Then comes the stage of concentration.
This component of the trance experience allows patients to have access or “turn
on” the traumatic memories during the psychotherapeutic session and then “shut
them off ” once the work has been done. During the final stage, the patient
comes to define herself or himself as being in control again.
The
underlying principle to remember is that the most damaging effect of
overwhelming trauma is that it renders its vic-tims defenseless. Because of the
lack of physical and emotional control, patients activate dissociative defenses
in an attempt to master their experiences. By using self-hypnosis, the
therapist can model and teach the patient to regain control over her or his
memories. Patients must be encouraged to remember as much as they feel is safe
to remember at a given time. The goal is that pa-tients learn how to think
about traumatic experiences, rather than negating their existence. The use of
self-hypnosis teaches patients that they are in control of their experiences.
Patients must dispel the magical beliefs that therapists “can take away the
memories”. Rather, by modeling this sense of trust in their therapists,
patients learn to trust themselves. They relearn trust in their own feelings
and perceptions.
The challenge in treating victims of abuse is to achieve a new sense of unity within the patient after the initial fragmentation caused by the traumatic experience. Overwhelming trauma tends to cause sudden and radical discontinuities in consciousness, which leaves the victims with a polarized view of themselves in-volving, on one hand the old self (before the trauma) and, on the other, the helpless, defenseless and traumatized victim. Our goal is to find ways to integrate these two aspects of the self. Here, the patient’s task is to acknowledge and place into perspective painful life events, thereby making them acceptable to conscious awareness.
One of
the advantages of the use of hypnosis is that the affect elicited can be so
powerful that most patients do not need to remember every single event of abuse
or trauma. In fact, through the use of hypnosis, the therapist may help the
patient consolidate the memories in a constructive way, thus facilitating
recovery. After a condensation of the traumatic experiences, patients become
ready to accept the victimized self. Instead of continuing the self-blame and
shame because of what happened to them, they can learn to acknowledge and even
thank themselves for what they did to survive. This restructuring allows them
to shift their perception of self, changing their self-image from that of a
victim to that of a survivor.
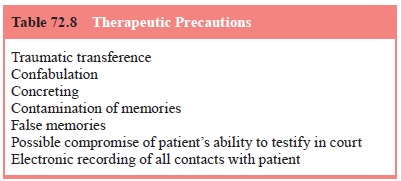
Therapeutic Precautions Therapeutic
precautions are shown in Table 72.8.
The strength of transference during the psycho-therapy of trauma victims is
enormous. The use of hypnosis does not prevent development of a transference
reaction; it may actually facilitate its emergence earlier than in regular
therapy owing to the intensity with which the material is expressed and
memories are recovered (Maldonado and Spiegel, 1994, 1995, 2002b).
Reliving
the traumatic experience along with the pa-tient may allow a special feeling of
“being there with them” at the moment of trauma. This allows the therapist to
provide guidance, support, protection and comfort as the patient goes through
the difficult path of reprocessing traumatic memo-ries. On the other hand, this
kind of traumatic transference
between the therapist and the victim of sexual assault is dif-ferent in the
sense that the feelings transferred are related not so much to early object
relationships but to the abuser or cir-cumstances that are associated with the
trauma (Spiegel, 1992). Instead of seeing this expressed anger at the therapist
as a form of negative transference reaction, we should explore the pos-sibility
that this may be a healthy attempt for the patient to ex-perience anger toward
the perpetrator. As therapists, we should not minimize or shut off these
feelings. This will only confirm the patient’s former perception that there was
something wrong with him or her for having these feelings, which will probably
activate further use of primitive defenses, including dissocia-tion or acting
out.
A more
serious complication of the use of hypnosis with trauma victims is the possible
creation of false memories.
Hypnosis, with its heightened sense of concentration, allows the patient to
focus intensely on a given time or place, en-hancing memory recall. The
principle of state-dependent memory also makes it plausible that the mere
entrance into this trance state can facilitate retrieval of memories associated
with a similar state of mind that may have occurred during the trauma and
subsequent flashbacks. However, not every mem-ory recovered with the use of
hypnosis is necessarily true. Hypnosis can facilitate improved recall of true
as well as con-fabulated material (Dywan and Bowers, 1983). Suggestibility is
increased in hypnosis, and information can be implanted or imagined and
reported as verdict (Laurence and Perry, 1983; McConkey, 1992). Because of
this, therapists are warned about “believing” everything a patient is able to
recall. Just as we use therapeutic judgment to analyze and interpret our
patients’ (nontraumatic) childhood memories, fantasies and dreams, so should we
treat hypnotically recovered material with caution.
To this
date, no evidence proves that the patient’s con-frontation with alleged
perpetrators of childhood abuse or pursuit of legal retribution toward the
perpetrator provides any therapeutic benefit. As therapists, we cannot be
certain of which memories are real, which are completely confabu-lated, and
which are a combination of both. Because of this, we should not encourage our
patients to take legal actions. If, on the other hand, our patients insist in
pursuing this avenue, it is our duty to warn them of our concerns but to be
support-ive of whatever final decision they make. Certainly we will do a
service to our patients if we inform them of all the legal ramifications that
the use of hypnosis, or any other form of memory enhancement, may have for
their defense, including their ability to testify in court or to use the
material recovered by such techniques.
Related Topics