Chapter: Essentials of Psychiatry: Antipsychotic Drugs
Antipsychotic Medications for Different Indications
Antipsychotic
Medications for Different Indications
Antipsychotic
agents are effective for treating nearly every medical and psychiatric
condition where psychotic symptom or aggression is the predominant feature. The
development of second-generation antipsychotics has been a major clinical
advance for the treatment of schizophrenia. At present, these second-generation
drugs are being used for schizophrenia as the first-line treatment, and are
being used increasingly for various conditions beyond schizophrenia as happened
with the first-generation anti-psychotics (Marder, 1997; Glick et al., 2001). The low incidence of EPS
and TD associated with second-generation agents is highly beneficial in several
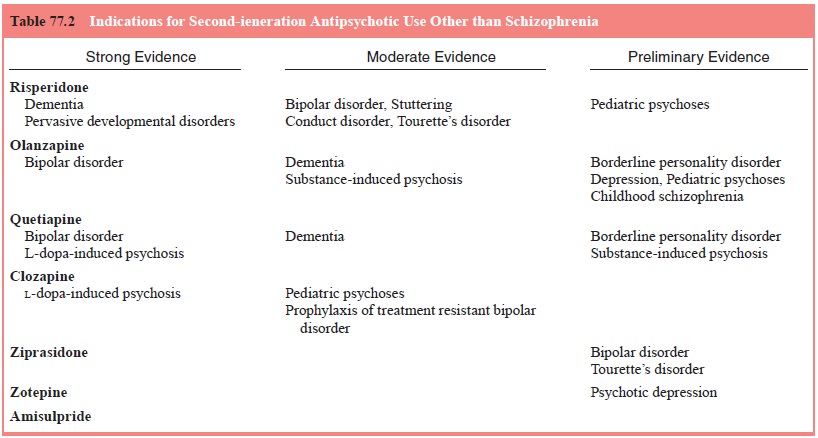
neuropsychiatric conditions. A summary of various indications for
second-generation antipsychotics is shown in Table 77.2. Some uses have gained
general acceptance, whereas others depend on moderate or preliminary evidence.
Schizophrenia and Schizoaffective Disorder
Nearly
all acute episodes of schizophrenia and schizoaffec-tive disorder, including
first episode psychosis and recurrence in chronic schizophrenia, should be treated
with antipsychotic medications (American Psychiatric Association, 2000). The
psy-chiatrist should evaluate the patient’s mental status and physical
condition before establishing a baseline for the administration of
antipsychotic medications. Once the patient is diagnosed, pharmacotherapy
should be applied as early in this phase as possible.
Continuous
medications may be preferable for most pa-tients with schizophrenia, even if
they are symptom free, to re-duce the likelihood of relapse.
Major Depression with Psychotic Features
Clear
psychotic symptoms, such as delusions or hallucinations, are observed in
approximately 25% of patients with major de-pressive disorder (Rothschild,
1996). These symptoms often respond poorly to antidepressants when they are
administered alone, and may require the use of adjunctive antipsychotic agents
(Marder, 1997). Conventional antipsychotic drugs are likely to expose patients
to the development of TD and EPS, which may occur more frequently in patients
with affective disorders than in those with schizophrenia (Casey, 1999). Thus,
second-generation antipsychotics may have a more beneficial effect for this
patient population.
There is
clinical evidence that some of the second-genera-tion antipsychotics may have
antidepressant effects in addition to their antipsychotic properties, and thus
may improve depres-sive symptoms in schizophrenia (Tollefson et al., 1999; Buckley, 2001). Although
depressive symptoms have traditionally been treated with antidepressants, a
number of case reports and open trials have shown risperidone and olanzapine to
be efficacious as monotherapy or adjunctive treatment for the treatment of
de-pression without psychotic features (Jacobsen, 1995; Ostroff and Nelson,
1999) (for review, see Buckley, 2001).
Mania
In almost
50% of manic episodes, clear psychotic symptoms, such as delusions or
hallucinations, are observed (Goodwin and Jamison, 1990). Antipsychotic
medications can effectively treat the symptoms of acute mania, particularly in
patients, who present with prominent agitation, in advance of the onset of
action of lithium or mood stabilizers (Marder, 1997; Buckley, 2001). Over the
past few years, second-generation antipsychotics have gained increasing favor
over the conventional neuroleptics for the treatment of bipolar disorder
because of their fewer EPS, a presumably lower risk of TD, and antimanic or
mood stabilizing effects (Thase and Sachs, 2000). Currently, second-generation
antipsychotics are being used as second-choice treatments for bipolar disorder
and/or adjunctive therapy with lithium, carbamazepine, or sodium valproate
(Ghaemi, 2000).
Tourette’s Disorder
Tourettes’s
disorder is a neurobehavioral disorder characterized clinically by motor and
vocal tics (Jimenez-Jimenez and Garcia-Ruiz, 2001). Tics are usually present in
childhood and may per-sist throughout life. The pathophysiology of the illness
is not well known. When the tics interfere with the functioning of the patient,
an antipsychotic medication can be effective in reduc-ing the severity of both
motor and vocal tics (Marder, 1997). Al-though haloperidol and pimozide have
been the most commonly used agents for the disease, second-generation
antipsychotics are considered as promising agents for the control of tics, because
of their better adverse event profiles.
Substance-related Disorders
A variety
of substances, including amphetamines, cocaine, alco-hol and phencyclidine, can
cause schizophrenia-like symptoms that occur while the patient is intoxicated
or during drug with-drawal (Marder, 1997). While clinical trials have not yet
estab-lished the efficacy of the second-generation antipsychotics for substance
use disorders, several case reports and open-labeled studies offer suggestions
of the effectiveness of new agents in these off-label uses (Misra and Kofoed,
1997; Smelson et al., 1997).
Behavioral Disturbances in the Elderly
Dementia,
whether due to Alzheimer’s disease or other causes, is frequently associated
with behavioral disturbance, agitation and psychotic phenomena (e.g.,
persecutory delusions, hallucinations) (Stoppe et al., 1999). The management of behavioral disturbance and
psychosis in the elderly is complicated by age-related decline in drug
metabolism, vulnerability to drug–drug interactions, high incidence of
concomitant physical illnesses and heightened sen-sitivity to EPS and TD
(Marder, 1997; Buckley, 2001). Usually, lower dosages are more necessary for
the elderly than for younger patients. Although evidence from a number of
double-blind stud-ies supports the efficacy of traditional antipsychotics for
treat-ing agitated elderly patients, the use of older agents is limited by EPS,
TD, anticholinergic adverse effects, sedation, and orthos-tatic hypotension,
which may result in falls and fractures.
Other Organic Syndromes
Patients
with Parkinson’s disease (PD) are sometimes accompa-nied with psychotic
symptoms. Second-generation antipsychot-ics can offer a true benefit to this
patient population (Friedman and Factor, 2000). Patients with Huntington’s disease
(HD) can also benefit from antipsychotic medications (Marder, 1997). As with
PD, the use of conventional agents worsens chorea move-ment disturbance
(Buckley, 2001).
Childhood Schizophrenia
Children
with schizophrenia may need neuroleptics for a long term. At present, no
controlled trials have been published on the use of risperidone, olanzapine,
quetiapine, or ziprasidone for the pediatric population with schizophrenia,
thus definitive evidence is lacking. A number of open clinical trials and case
reports of these new agents, however, indicate a possible effectiveness, though
pediatric patients seem to have a greater propensity than adults for side
effects, particularly EPS, weight gain and dyspho-ria, but also prolactin
increase and white blood count aberrations (Kumra et al., 1998; Toren et al.,
1998; Wudarsky et al., 1999;
McConville et al., 2000).
Related Topics