Chapter: Basic & Clinical Pharmacology : Clinical Use of Antimicrobial Agents
Antimicrobial Prophylaxis
ANTIMICROBIAL PROPHYLAXIS
Antimicrobial agents
are effective in preventing infections in many settings. Antimicrobial
prophylaxis should be used in circum-stances in which efficacy has been
demonstrated and benefits outweigh the risks of prophylaxis. Antimicrobial
prophylaxis may be divided into surgical prophylaxis and nonsurgical
prophylaxis.
Surgical Prophylaxis
Surgical wound
infections are a major category of nosocomial infections. The estimated annual
cost of surgical wound infections in the United States is $1.5 billion.
The National Research
Council (NRC) Wound Classification Criteria have served as the basis for
recommending antimicrobial prophylaxis. NRC criteria consist of four classes
[see Box: National Research Council (NRC) Wound Classification Criteria].
The
Study of the Efficacy of Nosocomial Infection Control (SENIC) identified four
independent risk factors for postopera-tive wound infections: operations on the
abdomen, operations lasting more than 2 hours, contaminated or dirty wound
classifi-cation, and at least three medical diagnoses. Patients with at least
two SENIC risk factors who undergo clean surgical procedures have an increased
risk of developing surgical wound infections and should receive antimicrobial
prophylaxis.
Surgical
procedures that necessitate the use of antimicrobial prophylaxis include
contaminated and clean-contaminated opera-tions, selected operations in which
postoperative infection may be catastrophic such as open heart surgery, clean
procedures that involve placement of prosthetic materials, and any procedure in
an immunocompromised host. The operation should carry a signifi-cant risk of
postoperative site infection or cause significant bacte-rial contamination.
General principles of
antimicrobial surgical prophylaxis include the following:
1. Theantibiotic
should be active against common surgical wound pathogens; unnecessarily broad
coverage should be avoided.
2.
The antibiotic should have proved efficacy in clinical trials.
3. The antibiotic must
achieve concentrations greater than the MIC of suspected pathogens, and these
concentrations must be present at the time of incision.
4. The shortest
possible course—ideally a single dose—of the most effective and least toxic
antibiotic should be used.
5. The newer
broad-spectrum antibiotics should be reserved for therapy of resistant
infections. If all other factors are equal, the least expensive agent should be
used.
The proper selection
and administration of antimicrobial pro-phylaxis are of utmost importance.
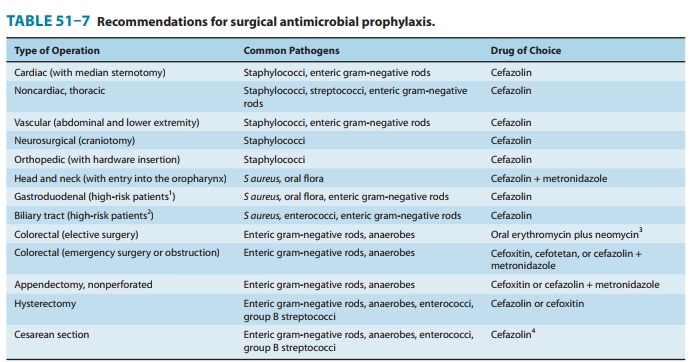
Common indications for sur-gical prophylaxis are shown in Table 51–7. Cefazolin
is the prophylactic agent of choice for head and neck, gastroduodenal, biliary
tract, gynecologic, and clean procedures. Local wound infection patterns should
be considered when selecting antimicro-bial prophylaxis. The selection of
vancomycin over cefazolin may be necessary in hospitals with high rates of
methicillin-resistant Saureus or S epidermidis infections. The
antibiotic should be presentin adequate concentrations at the operative site
before incision and throughout the procedure; initial dosing is dependent on
the volume of distribution, peak levels, clearance, protein binding, and
bioavailability. Parenteral agents should be administered dur-ing the interval
beginning 60 minutes before incision; administra-tion up to the time of
incision is preferred. In cesarean section, the antibiotic is administered
after umbilical cord clamping. If short-acting agents such as cefoxitin are
used, doses should be repeated if the procedure exceeds 3–4 hours in duration.
Single-dose pro-phylaxis is effective for most procedures
and results in decreased toxicity and antimicrobial resistance.Improper
administration of antimicrobial prophylaxis leads to excessive surgical wound
infection rates. Common errors in anti-biotic prophylaxis include selection of
the wrong antibiotic,
National Research Council (NRC) Wound
Classification Criteria
Clean: Elective, primarily closed procedure; respiratory,
gas-trointestinal, biliary, genitourinary, or oropharyngeal tract not entered;
no acute inflammation and no break in technique; expected infection rate ≤ 2%.
Clean contaminated: Urgent or emergency case that is oth-erwise clean; elective,
controlled opening of respiratory, gas-trointestinal, biliary, or oropharyngeal
tract; minimal spillage or minor break in technique; expected infection rate ≤ 10%.
Contaminated: Acute nonpurulent inflammation; majortechnique break or major
spill from hollow organ; penetrat-ing trauma less than 4 hours old; chronic
open wounds to be grafted or covered; expected infection rate about 20%.
Dirty: Purulence or abscess; preoperative perforation ofrespiratory, gastrointestinal, biliary, or oropharyngeal tract; penetrating trauma more than 4 hours old; expected infec-tion rate about 40%.
Nonsurgical Prophylaxis
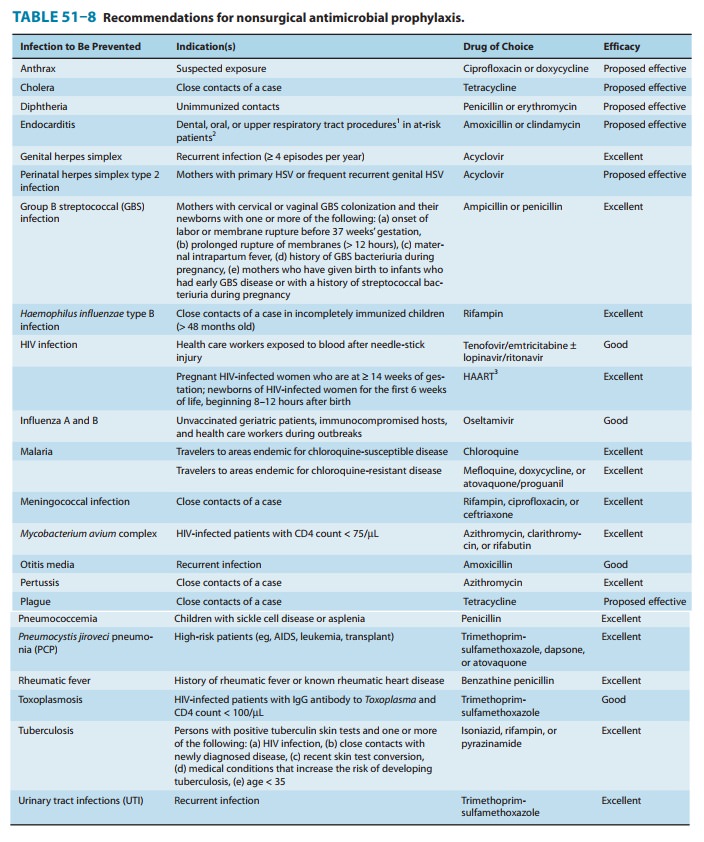
Nonsurgical
prophylaxis includes the administration of antimicro-bials to prevent
colonization or asymptomatic infection as well as the administration of drugs
following colonization by or inocula-tion of pathogens but before the
development of disease. Nonsurgical prophylaxis is indicated in individuals who
are at high risk for temporary exposure to selected virulent pathogens and in
patients who are at increased risk for developing infection because of
under-lying disease (eg, immunocompromised hosts). Prophylaxis is most
effective when directed against organisms that are predictably sus-ceptible to
antimicrobial agents. Common indications and drugs for nonsurgical prophylaxis
are listed in Table 51–8.
Related Topics