Chapter: Essentials of Psychiatry: Eating Disorders
Anorexia Nervosa: Differential Diagnosis
Differential
Diagnosis
Although
depression, schizophrenia and obsessive–compulsive disorder may be associated
with disturbed eating and weight loss, it is rarely difficult to differentiate
these disorders from anorexia nervosa. Individuals with major depression may
lose significant amounts of weight but do not exhibit the relentless drive for
thin-ness characteristic of anorexia nervosa. In schizophrenia, starva-tion may
occur because of delusions about food, for example, that it is poisoned.
Individuals with obsessive–compulsive disorder may describe irrational concerns
about food and develop rituals related to meal preparation and eating but do
not describe the intense fear of gaining weight and the pervasive wish to be
thin that characterize anorexia nervosa.
A wide
variety of medical problems cause serious weight loss in young people and may
at times be confused with anorexia nervosa. Examples of such problems include
gastric outlet ob-struction, Crohn’s disease and brain tumors. Individuals
whose weight loss is due to a general medical illness generally do not show the
drive for thinness, the fear of gaining weight and the increased physical
activity characteristic of anorexia nervosa. However, the psychiatrist is well
advised to consider any chronic medical illness associated with weight loss,
especially when evaluating individuals with unusual clinical presentations such
as late age at onset or prominent physical complaints, for exam-ple, pain and
gastrointestinal cramping while eating.
Course and Natural History
The
course of anorexia nervosa is enormously variable. Some in-dividuals have mild
and brief illnesses and either never come to medical attention or are seen only
briefly by their pediatrician or general medical physician. It is difficult to
estimate the frequency of this phenomenon because such individuals are rarely
studied.
Most of
the literature on course and outcome is based on individuals who have been
hospitalized for anorexia nervosa. Although such individuals presumably have a
relatively severe illness and adverse outcomes, a substantial fraction,
probably between one-third and one-half, make full and complete psy-chological
and physical recoveries. On the other hand, anorexia nervosa is also associated
with an impressive long-term mortal-ity. The best data currently available
suggest that 10 to 20% of patients who have been hospitalized for anorexia nervosa
will, in the next 10 to 30 years, die as a result of their illness. Much of the
mortality is due to severe and chronic starvation, which eventu-ally terminates
in sudden death. In addition, a significant fraction of patients commit
suicide.
Between these
two extremes are a large number of indi-viduals whose lives are impaired by
persistent difficulties with eating. Some are severely affected maintaining a
chronic state of semistarvation, bizarre eating rituals and social isolation;
others may gain weight but struggle with bulimia nervosa and strict rules about
food and eating; and still others may recover initially but then relapse into
another full episode. There is a high fre-quency of depression among
individuals who have had anorexia nervosa and a significant frequency of drug
and alcohol abuse, but psychotic disorders develop only rarely. Thus, in
general, in-dividuals either recover or continue to struggle with
psychologi-cal and behavioral problems that are directly related to the eating
disorder. It is of note that it is rare for individuals who have had anorexia
nervosa to become obese.
It is
difficult to specify factors that account for the vari-ability of outcome in
anorexia nervosa. A significant body of experience suggests that the illness
has a better prognosis whenit begins in adolescence, but there are also
suggestions that pre-pubertal onset may portend a difficult course. It is
likely that the severity of the illness (e.g., the lowest weight reached, the
number of hospitalizations) and the presence of associated symptoms, such as
binge-eating and purging, also contribute to poor out-come. However, it is
impossible to predict course and outcome in an individual with any certainty.
Goals of Treatment
The first
goal of treatment is to engage the patient and her or his family. For most
patients with anorexia nervosa, this is chal-lenging. Patients usually minimize
their symptoms and suggest that the concerns of the family and friends, who
have often been instrumental in arranging the consultation, are greatly
exag-gerated. It is helpful to identify a problem that the patient can
acknowledge, such as weakness, irritability, difficulty concen-trating, or
trouble with binge-eating. The psychiatrist may then attempt to educate the
patient regarding the pervasive physical and psychological effects of
semistarvation and about the need for weight gain if the acknowledged problem
is to be successfully addressed.
A second
goal of treatment is to assess and address acute medical problems, such as fluid
and electrolyte disturbances and cardiac arrhythmias. Depending on the severity
of illness, this may require the involvement of a general medical physician.
The additional but most difficult and time-consuming goals are the restoration
of normal body weight, the normalization of eating and the resolution of the
associated psychological disturbances. The final goal is the prevention of
relapse.
Treatment
A common
major impediment to the treatment of patients with anorexia nervosa is their
disagreement with the goals of treat-ment; many of the features of their
illness are simply not viewed by patients as a problem. In addition, this may
be compounded by a variety of concerns of the patient, such as basic mistrust
of relationships, feelings of vulnerability and inferiority, and sen-sitivity
to perceived coercion. Such concerns may be expressed through considerable
resistance, defiance, or pseudocompliance with the psychiatrist’s interventions
and contribute to the power struggles that often characterize the treatment
process. The psy-chiatrist must try to avoid colluding with the patient’s
attempts to minimize problems but at the same time allow the patient enough
independence to maintain the alliance. Dealing with such dilem-mas is
challenging and requires an active approach on the part of the psychiatrist. In
most instances, it is possible to preserve the alliance while nonetheless
adhering to established limits and the need for change.
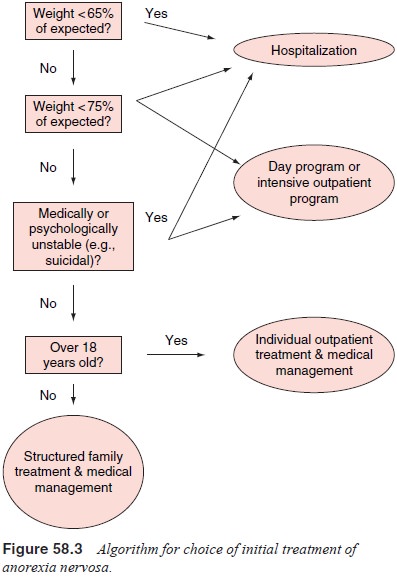
The
initial stage of treatment should be aimed at reversing the nutritional and
behavioral abnormalities (Figure 58.3). The intensity of the treatment required
and the need for partial or full hospitalization should be determined by the
current weight, the rapidity of weight loss, and the severity of associated
medical and behavioral problems and of other symptoms such as depression. In
general, patients whose weights are less than 75% of expected should be viewed
as medically precarious and require intensive treatment such as
hospitalization.
Most
inpatient or day treatment units experienced in the care of patients with
anorexia nervosa use a structured treatment approach that relies heavily on
supervision of calorie intake by the staff. Patients are initially expected to
consume sufficient cal-ories to maintain weight, usually requiring 1500 to 2000
kcal/day
in four
to six meals. After the initial medical assessment has been completed and
weight has stabilized, calorie intake is gradually increased to an amount
necessary to gain 2 to 5 lb/week. Because the consumption of approximately 4000
kcal beyond mainte-nance requirements is needed for each pound of weight gain,
the daily calorie requirements become impressive, often in the range of 4000
kcal/day. Some eating disorder units provide only food while others rely on
nutritional supplements such as Ensure or Sustacal. During this phase of
treatment it is necessary to moni-tor patients carefully; many will resort to
throwing food away or vomiting after meals. Careful supervision is also
required to obtain accurate weights; patients may consume large amounts of
fluid before being weighed or hide heavy articles under their clothing.
During
the weight restoration phase of treatment patients require substantial
emotional support. It is probably best to ad-dress fears of weight gain with
education about the dangers of semistarvation and with the reassurance that
patients will not be allowed to gain “too much” weight. Most eating disorders
units impose behavioral restrictions, such as limits on physical activ-ity,
during the early phase of treatment. Some units use an ex-plicit behavior
modification regimen in which weight gain is tied to increased privileges and
failure to gain weight results in bed rest.
A
consistent and structured treatment approach, with or without an explicit
behavior modification program, is generally successful in promoting weight
recovery but requires substantial energy and coordination to maintain a
supportive and nonpunitivetreatment environment. In most experienced treatment
units, parenteral methods of nutrition, such as nasogastric feeding or
intravenous hyperalimentation, are only rarely needed. Nutri-tional counseling
and behavioral approaches can also be effec-tive in helping patients expand
their dietary repertoire to include foods they have been frightened of
consuming.
As weight
increases, individual, group and family psycho-therapy can begin to address
other issues in addition to the dis-tress engendered by gaining weight. For
example, it is typically important for patients to recognize that they have
come to base much of their self-esteem on dieting and weight control and are
likely to judge themselves according to harsh and unforgiving standards.
Similarly, patients should be helped to see how the eating disorder has interfered
with the achievement of personal goals such as education, sports, or making
friends.
There is,
present, no general agreement about the most useful type of psychotherapy or
the specific topics that need to be addressed. Most eating disorders programs
employ a variety of psychotherapeutic interventions. A number of psychiatrists
recommend the use of individual and group psychotherapy us-ing
cognitive–behavioral techniques to modify the irrational overemphasis on
weight. Although most authorities see little role for traditional
psychoanalytic therapy, individual and group psychodynamic therapy can address
such problems as insecure attachment, separation and individuation, sexual
relationships and other interpersonal concerns. There is good evidence sup-porting
the involvement of the family in the treatment of younger patients with
anorexia nervosa. Family therapy can be helpful in addressing family members’
fears about the illness; interventions typically emphasize parental
cooperation, mutual support and consistency, and establishing boundaries
regarding the patient’s symptoms and other aspects of his or her life.
Despite
the multiple physiological disturbances associ-ated with anorexia nervosa,
there is no clearly established role for medication. The earliest systematic
medication trials in ano-rexia nervosa focused on the use of neuroleptics.
Theoretically, such agents might help to promote weight gain, to reduce
physi-cal activity and to diminish the distorted thinking about shape and
weight, which often reaches nearly delusional proportions. Early work in the
late 1950s and 1960s using chlorpromazine led to substantial enthusiasm, but
two placebo-controlled trials of the neuroleptics, sulpiride and pimozide, were
unable to establish significant benefits. In recent years interest has grown in
taking advantage of the impressive weight gain associated with some atypical
antipsychotics; however, no controlled data supporting this intervention have
yet appeared. Despite the frequency of de-pression among patients with anorexia
nervosa, there is no good evidence supporting the use of antidepressant
medication in their treatment.
Unfortunately,
although controlled trials have provided some evidence of benefit, the impact
of cyproheptadine, an anti-histamine, in anorexia nervosa appears limited.
A large
percentage of patients with anorexia nervosa re-main chronically ill; 30 to 50%
of patients successfully treated in the hospital require rehospitalization
within 1 year of discharge. Therefore, posthospitalization outpatient
treatments are recom-mended to prevent relapse and improve overall short- and
long-term functioning. Several studies have attempted to evaluate the efficacy
of various outpatient treatments for anorexia nervosa including behavioral,
cognitive–behavioral and supportive psy-chotherapy, as well as a variety of
nutritional counseling inter-ventions. Although most of these treatments seem
to be helpful the clearest findings to date support two interventions. For
pa-tients whose anorexia nervosa started before age 18 years and who have had
the disorder for less than 3 years, family therapy is effective, and for adult
patients, cognitive–behavioral therapy reduces the rate of relapse. Preliminary
information suggests that fluoxetine treatment may reduce the risk of relapse
among patients with anorexia nervosa who have gained weight, but ad-ditional
controlled data are required to document the usefulness of this intervention.
Refractory Patients
Some
patients with anorexia nervosa refuse to accept treatment and thereby can raise
difficult ethical issues. If weight is ex-tremely low or if there are acute
medical problems, it may be ap-propriate to consider involuntary commitment.
For patients who are ill but more stable, the psychiatrist must weigh the
short-term utility of involuntary treatment against the disruption of a
poten-tial alliance with the patient.
The goals of treatment may need to be modified for patients with chronic illness who have failed multiple previous attempts at inpatient and outpatient care. Treatment may be appropriately aimed at preventing further medical, psychological and social de-terioration in the hope that the anorexia nervosa may eventually improve with time.
Related Topics