Chapter: Clinical Anesthesiology: Anesthetic Management: Anesthesia for Trauma & Emergency Surgery
Anesthesia for Traumatic Brain Injury
TRAUMATIC BRAIN INJURY
Any trauma patient with altered level of
con-sciousness must be considered to have a traumatic brain injury (TBI) until
proven otherwise . The presence or suspicion of a TBI mandates attention to
maintaining cerebral perfu-sion and arterial oxygenation during all aspects of
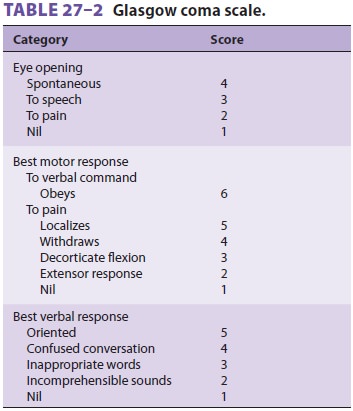
care. The most reliable clinical assessment tool in determining the significance
of TBI in a nonse-dated, nonparalyzed patient is the Glasgow coma scale (GCS,
Table 27–2). A declining motor score is suggestive of progressing neurological
deteriora-tion, prompting urgent neurosurgical evaluation and possible surgical
intervention. Although trauma patients frequently have head injuries, few head
inju-ries require emergent neurosurgical intervention.
TBIs are categorized as either primary or sec-ondary. Primary brain injuries are usually focal inju-ries
directly related to trauma, disrupting normal anatomy or physiology, or both.
Four categories of primary brain injury are seen: (1) subdural hematoma; (2)
epidural hematoma; (3) intraparen-chymal hemorrhage; and (4) nonfocal, diffuse
neu-ronal injury disrupting axons of the central nervous system. These injuries
potentially compromise cere-bral blood flow and elevate intracranial
pressure (ICP). Death occurring soon after
significant head trauma is usually a result of the primary brain injury.
Acute subdural hematoma is the most com-mon
condition warranting emergency neurosurgery and is associated with the
highest mortality. Small bridging veins between the skull and brain are
disrupted in deceleration or blunt force inju-ries, resulting in blood
accumulation and compres-sion of brain tissue. The accumulation of blood raises
ICP and compromises cerebral blood flow. Morbidity and mortality are related to
the size of the hematoma and magnitude of the midline shift of intracranial
contents. Midline shifts of intracra-nial contents may exceed the size of the
hematoma, suggesting a significant contribution of cerebral edema. Acute
subdural hematomas should be sur-gically evacuated, particularly in patients
with ele-vated ICP.
Epidural
hematoma occurs when the middlecerebral artery or other
cranial vessels are disrupted, most often in association with a skull fracture.
This injury accounts for less than 10% of neurosurgi-cal emergencies and has a
much better prognosis than acute subdural hematoma. The patient with an
epidural hematoma may initially be conscious-ness, followed by progressive
unresponsiveness and coma. Emergent surgical decompression is indi-cated when
supratentorial lesions occupy more than 30 mL volume and infratentorial lesions
occupy more than 10 mL volume (brainstem compression may occur at much lower
hematoma volumes). A small epidural hematoma may not require imme-diate
evacuation if the patient is neurologically intact, if close observation and
repeated neurologi-cal examinations are possible, and if neurosurgical resources
are available should emergent decompres-sion become necessary.
Intraparenchymal
injuries are caused by rapiddeceleration of the brain
within the skull, usu-ally involving the tips of the frontal or temporal lobes.
They represent nearly 20% of neurosurgical emergencies following trauma. These
injuries tend to be associated with signif icant edema, necrosis, and infarcts
in the tissue surrounding the dam-aged tissue. Intraparenchymal injury may
coexist with a subdural hematoma. There is no consensus regarding the surgical
interventions that should be performed for intraparenchymal hemorrhage, but
surgical decompression may be necessary to reduce dangerously sustained
increased ICP.
Diffuse neuronal injury results from events
resulting in rapid deceleration or movement of the brain tissue of sufficient
force to disrupt neurons and axons. This form of brain injury is more common in
children than in adults. The extent of the injury may not be obvious in the
period soon after injury but will become apparent with serial clinical and
radiographic (magnetic resonance imaging) exami-nations. The greater the extent
of diffuse neuronal injury following trauma, the higher will be the mor-tality
and severe disability. Surgical interventions are not indicated for these
injuries unless a decompres-sive craniectomy is required for relief of
refractory elevated ICP .
Secondary brain injuries are considered
poten-tially preventable injuries. Systemic hypotension (systolic blood
pressures <90 mm Hg), hypoxemia (Pao2<60 mm Hg), hypercapnia
(Paco2>50 mm Hg), and hyperthermia (temperature >38.0°C) have a negative
impact on morbidity and mortality following head injuries, likely because of
their contributions to increasing cerebral edema and ICP. Hypotension and
hypoxia are recognized as major contributors to poor neurological recov-ery
from severe TBI. Hypoxia is the single most important parameter correlating to
poor neuro-logical outcomes following head trauma and should be corrected at
the earliest possible opportunity. Hypotension (mean arterial blood pressure <60 mm Hg) should also be
treated aggressively, using fluid or vasopressors, or both, to assure cere-bral
perfusion.
Management Considerations
A. Intracranial Pressure
In the absence of a clot requiring
evacuation, medi-cal interventions are the primary means of treating elevated
ICP following head trauma. Normal cerebral perfusion pressure (CPP), the
difference between mean arterial pressure
and ICP (ie, MAP − ICP CPP), is approximately 10 mm Hg. ICP monitoring
is not required for conscious and alert patients; in addi-tion, patients who
are intentionally anticoagulated or who have bleeding diathesis in response to
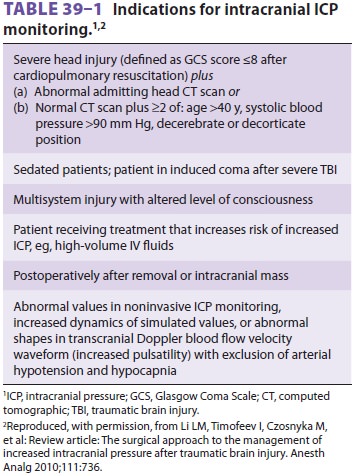
trauma should not have ICP monitoring. However, an ICP monitor should be placed
when serial neurological examinations and additional clinical assessments
reveal impairment, or when there is an increased risk for elevated ICP (Table
39–1). Interventions to reduce ICP are indicated when readings are higherthan
20–25 mm Hg. Although multiple studies have evaluated interventions aimed at
improving CPP and managing ICP without finding obvious outcomes benefit for any
treatment scheme, current Brain Trauma Foundation guidelines recommend
maintaining CPP between 50 and 70 mm Hg and ICP at less than 20 mm Hg for
patients with severe head injury.
Cerebral blood flow is related to arterial
car-bon dioxide concentration in a dose-dependent relationship. As arterial
carbon dioxide levels decrease, cerebral vasoconstriction occurs, reduc-ing
ICP. Conversely, as arterial carbon dioxide levels rise, cerebral vasodilation
occurs, increasing ICP. Changes in arterial carbon dioxide levels exert a
prompt cerebral blood flow and ICP response, mak-ing hyperventilation an
effective intervention when brain herniation is suspected or proven. However,
this intervention must be appreciated in the context of TBI: hyperventilation
in the presence of systemic hypotension increases the risk of neurological
isch-emia and should be avoided in the early stages of resuscitation for
patients with TBI.
Osmotic
diuretic therapy is another com-monly
used and widely accepted method for reduc-ing elevated ICP. Intravenous
mannitol doses of 0.25–1.0 g/kg body weight are effective in draw-ing
intravascular fluid into the vascular system. As extravascular fluid is drawn
into the vascular sys-tem, brain edema and ICP will decrease. Because this
intervention is very effective for inducing brisk diuresis, serum osmolarity
and electrolytes (particu-larly potassium) must be monitored.
Barbiturate
coma is an intervention thatattempts to decrease
cerebral metabolic rate, cerebral blood flow, and cerebral oxygen demand in
order to reduce elevated ICP and suppress the metabolic rate of ischemic cells
until cerebral perfusion improves. Hypotension is commonly associated with this
ther-apy, which should limit its use in the hemodynami-cally unstable patient.
Vasopressors may be used in order to maintain CPP between 50 and 70 mm Hg. The
pentobarbital dose administered is based upon electroencephalographic evidence of
burst suppres-sion in order to maximally reduce the cerebral meta-bolic rate of
oxygen.
B. Severe TBI & Multiple Trauma
The presence of a severe head injury in the pres-ence of other major
traumatic injuries and ongo-ing hemorrhage creates a situation in which patient
management goals may conflict. As noted above, in the head-injured patient
requiring emergent decompression, mean blood pressures must be maintained
between 50 and 70 mmHg to assure adequate CPP and prevention of secondary
isch-emic neurological injuries. In patients without brain injury, hemorrhage
is usually treated with a more hypotensive goal until bleeding is controlled.
Deference is paid to the most life-threatening condition as the priority
intervention with the expectation that CPP be maintained throughout, even if
this approach results in greater transfusion requirements.
Related Topics