Chapter: Clinical Anesthesiology: Anesthetic Management: Anesthesia for Trauma & Emergency Surgery
Anesthesia for Primary Survey
PRIMARY SURVEY
Airway
Increasingly, emergency medical technician–
paramedics and flight nurses are trained to intu-bate patients in the
prehospital environment. More providers capable of airway management in the
critically ill or injured patient are now available to intervene in the
hospital setting as well. As a result, the anesthesiologist’s role in providing
initial trauma resuscitation has diminished in North America. This also means
that when called upon to assist in airway management in the emergency
department, anes-thesia providers must expect a challenging airway, as routine
airway management techniques likely have already proved unsuccessful.
There are three important aspects of airway management in the initial evaluation
of a trauma patient: (1) the need for basic life support; (2) the presumed
presence of a cervical spinal cord injuryuntil proven otherwise; and (3) the
potential for failed tracheal intubation. Effective basic
life support prevents hypoxia and hypercapnia from contributing to the
patient’s depressed level of consciousness. When hypercarbia produces a
depressed level of consciousness, basic airway
interventions oftenlessen the
need for endotracheal
intubation asarterial carbon
dioxide levels return to normal.
Finally, all trauma patients should be pre-sumed to have “full” stomachs
and an increased risk for pulmonary aspiration
of gastric contents. Assisted ventilation should be performed with vol-umes
sufficient to provide chest rise. Some clinicians will apply cricoid pressure,
although the efficacy of this maneuver is controversial.
Cervical spine injury is presumed in any
trauma patient complaining of neck pain, orwith any significant head injury,
neurological signs or symptoms suggestive of cervical spine injury, or
intoxication or loss of consciousness. The applica-tion of a cervical collar
(“C-collar”) before trans-port to protect the cervical spinal cord will limit
the degree of cervical extension that is ordinarily expected for direct
laryngoscopy and tracheal intu-bation. Alternative devices (eg,
videolaryngoscopes, fiberoptic bronchoscopes) should be immediately available.
The front portion of the C-collar can be removed to facilitate tracheal
intubation as long as the head and neck are maintained in neutral posi-tion by
a designated assistant maintaining manual in-line stabilization.
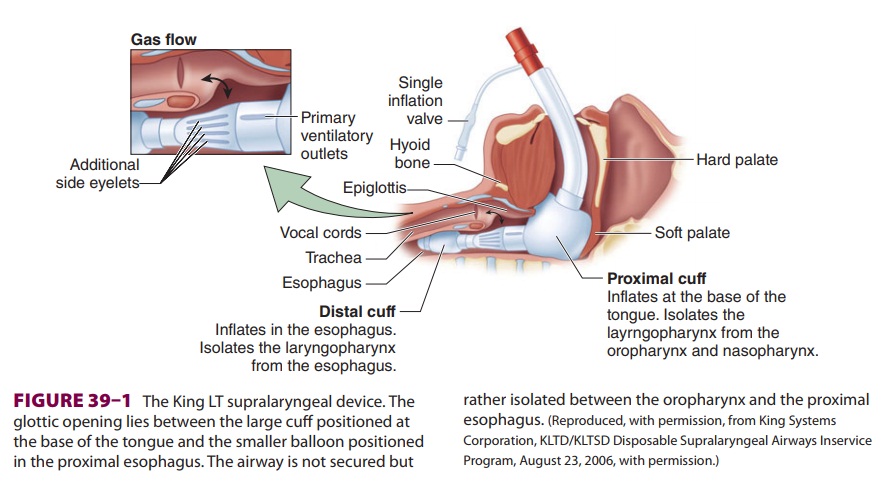
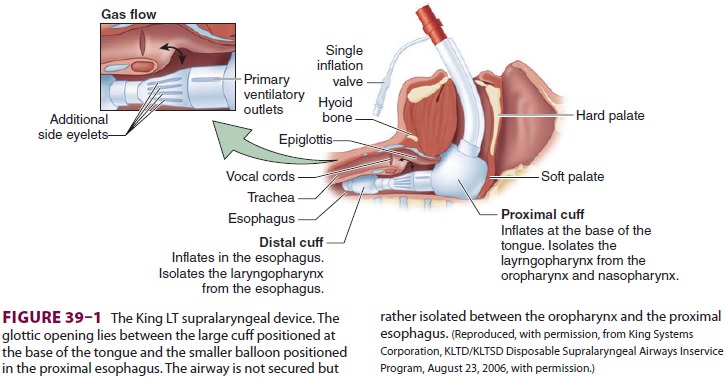
Alternative devices for airway management
(eg, esophageal–tracheal Combitube, King supra-laryngeal device) may be used if
direct laryngos-copy has failed, or in the prehospital environment. These
devices, blindly placed into the airway, isolate the glottic opening between a
large inflatable cuff positioned at the base of the tongue and a distal cuff
that most likely rests in the proximal esopha-gus (Figure 39–1). The prolonged presence of these devices in the airway has been
associated with glos-sal engorgement resulting from the large, proximal cuff
obstructing venous outflow from the tongue, and in some cases, tongue
engorgement has been sufficiently severe to warrant tracheostomy prior to their
removal. There is limited evidence that pre-hospital airway management in
trauma patients improves patient outcomes; however, failed tracheal intubation
in the prehospital environment certainly exposes patients to significant
morbidity.
Airway management of the trauma patient is uneventful in most
circumstances, and
cricothyroidotomy or tracheostomy is rarely required to secure the
trauma airway. When trauma significantly alters or distorts the facial or upper
airway anatomy to the point of impeding adequate mask ventilation, or when
hemorrhage into the air-way precludes the patient from lying supine, elective
cricothyroidotomy or tracheostomy should be con-sidered before any attempts are
made to anesthetize or administer neuromuscular blocking agents to the patient
for orotracheal intubation.
Breathing
In the multiple-injury patient, providers
should maintain a high level of suspicionfor pulmonary injury that could evolve
into a ten-sion pneumothorax when mechanical ventilation is initiated.
Attention must be paid to peak inspi-ratory pressure and tidal volumes
throughout the initial resuscitation. Pulmonary injury may not be immediately
apparent upon the patient’s arrival at the hospital, and abrupt cardiovascular
collapse shortly after instituting mechanical ventilation may announce the
presence of a pneumothorax. This should be managed by disconnecting the patient
from mechanical ventilation and performing bilat-eral needle
thoracostomy (accomplished by insert-ing a 14-gauge intravenous catheter into
the second interspace in the midclavicular line), and then by thoracostomy tube
insertion. Inspired oxygen con-centrations of 100% are used routinely in this
early phase of resuscitation.
Circulation
During the primary trauma patient survey,
signs of a pulse and blood pressure are sought. Unless the trauma patient
arrives at the hospital other than by ambulance, the resuscitation team will
likely have received information about the patient’s vital signs from the
prehospital personnel (emergency medi-cal technicians, flight nurses). The
absence of a pulse following trauma is associated with dismal chances of
survival. The ACS Committee on Trauma no lon-ger endorses the use of emergency
thoracotomy in treating patients without blood pressure or palpable pulse
following blunt trauma, even in the
presence of organized cardiac activity, given the lack of evidence supporting
survival following this intervention.Retrospective review of emergency
thoracotomy in Europe failed to demonstrate resuscitation benefit of this
procedure following either blunt or penetrating trauma in the setting of
cardiac arrest. In the setting of chest trauma without detectable blood
pressure or palpable pulse, current practice supports reserving resuscitative
thoracotomy for patients who experi-ence penetrating
trauma and have preserved, orga-nized cardiac rhythms or other signs of life.
In light of these recommendations, prompt placement of bilateral chest
tubes and adminis-tration of a 500–1000 mL fluid bolus should be implemented in
the pulseless victim of penetrating trauma. If return of spontaneous
circulation does not occur promptly, more aggressive interventions are not
indicated and resuscitation efforts can be terminated.
Neurological Function
Once the presence of circulation is
confirmed, a brief neurological examination is conducted. Level of
con-sciousness, pupillary size and reaction, lateralizing signs suggesting
intracranial or extracranial inju-ries, and indications of spinal cord injury
are quickly evaluated. As noted earlier, hypercarbia often causes depressed
neurological responsiveness following trauma; it is effectively corrected with
basic life sup-port interventions. Additional causes of depressed neurological
function—eg, alcohol intoxication, effects of illicit or prescribed
medications, hypogly-cemia, hypoperfusion, or brain or spinal injury— must also
be addressed. Mechanisms of injury must be considered as well as exclusion of other
factors in determining the risk for central nervous system trauma. Persistently
depressed levels of conscious-ness should be considered a result of central
nervous system injury until disproved by diagnostic studies.
Injury Assessment:Minimizing Risks of Exposure
The patient must be fully exposed and examined in order to adequately
assess the extent of injury, and this physical exposure increases the risk of
hypo-thermia. The presence of shock and intravenous fluid therapy also place
the trauma patient at great risk for developing hypothermia. As a result, the
resuscitation bay must be maintained at near body temperature, all fluids
should be warmed during administration, and the use of forced air patient
warmers, either below or covering the patient, should be utilized.
Related Topics