Chapter: Clinical Anesthesiology: Anesthetic Management: Anesthesia for Neurosurgery
Anesthesia for Head Trauma
Anesthesia for Head Trauma
Head injuries are a contributory factor in up to 50% of deaths
due to trauma. Most patients with head trauma are young, and many (10% to 40%)
have associated intraabdominal or intrathoracic injuries, long bone fractures,
and/or spinal inju-ries. The outcome from a head injury is dependent not only
on the extent of the neuronal damage at the time of injury, but also on the
occurrence of any secondary insults. These additional insults include: (1)
systemic factors such as hypoxemia, hypercapnia, or hypotension; (2) formation
and expansion of an epidural, subdural, or intracerebral hematoma; and (3)
sustained intracranial hyper-tension. Surgical and anesthetic management of
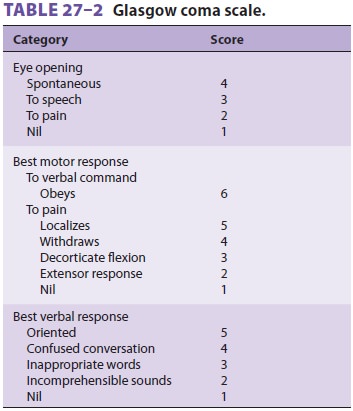
these patients is directed at preventing these sec-ondary insults. The Glasgow Coma Scale (GCS)
score (Table 27–2) generally correlates well with the severity of injury and outcome. A GCS score of 8 or less on admission is associated
with approxi-mately 35% mortality. Evidence of greater than a 5-mm midline
shift (on imaging) and ventricular compression on imaging are associated with
sub-stantially increased morbidity.
Specific lesions include skull
fractures, sub-dural and epidural hematomas, brain contusions (including
intracerebral hemorrhages), penetrating head injuries, and traumatic vascular
occlusions and dissections. The presence of a skull fracture greatly increases
the likelihood of an intracranial lesion. Linear skull fractures are commonly
associated
with subdural or epidural hematomas.
Basilar skull fractures may be associated with CSF rhinorrhea, pneumocephalus,
cranial nerve palsies, or even a cavernous sinus–carotid artery fistula.
Depressed skull fractures often present with an underlying brain contusion.
Contusions may be limited to the surface of the brain or may involve hemorrhage
in deeper hemispheric structures or the brainstem. Deceleration injuries often
produce both coup (fron-tal) and contrecoup (occipital) lesions. Epidural and
subdural hematomas can occur as isolated lesions, as well as in association with
cerebral contusions (more commonly with subdural than epidural lesions).
Operative treatment is usually elected
for depressed skull fractures; evacuation of epidural, subdural, and some
intracerebral hematomas; and debridement of penetrating injuries. Decompressive
craniectomy is used to provide room for cerebral swelling. The cranium is
subsequently reconstructed following resolution of cerebral edema.
ICP monitoring is usually indicated in patients with lesions
associated with intracranial hyperten-sion: large contusions, mass lesions,
intracerebral hemorrhage, or evidence of edema on imaging studies. ICP
monitoring should also be considered in patients with signs of intracranial
hypertension who are undergoing nonneurological procedures. Intracranial hypertension
should be treated with moderate hyperventilation, mannitol, pentobar-bital, or
propofol Studies suggest that sustained increases in ICP of greater than 60 mm
Hg result in severe disability or death. Unlike treatment fol-lowing spinal
cord trauma, multiple randomized trials have failed to detect the efficacy of
early use of large doses of glucocorticoids in patients with head trauma.
PREOPERATIVE MANAGEMENT
Anesthetic care of patients with severe
head trauma begins in the emergency department. Measures to ensure patency of
the airway, adequacy of ventila-tion and oxygenation, and correction of
systemic hypotension should go forward simultaneously with neurological and
trauma surgical evaluation. Airway obstruction and hypoventilation are common. Up
to 70% of such patients have hypoxemia, which may be complicated by pulmonary
contusion, fat emboli, or neurogenic pulmonary edema. The latter is attrib-uted
to marked systemic and pulmonary hyper-tension secondary to intense sympathetic
nervous system activity. Supplemental oxygen should be given to all patients
while the airway and ventilation are evaluated. All patients must be assumed to
have a cervical spine injury (up to 10% incidence) until the contrary is proven
radiographically. Patients with obvious hypoventilation, an absent gag reflex,
or a persistent score below 8 on the GCS (Table 27–2) require tracheal
intubation and hyperventilation. All other patients should be carefully
observed for deterioration.
Intubation
All patients should be regarded as having a full stomach and
should have cricoid pressure applied during ventilation and tracheal
intubation. In-line stabilization should be used during airway manip-ulation to
maintain the head in a neutral position,
unless radiographs confirm that there is no cervicalspine injury. Following
preoxygenation and hyper-ventilation by mask, the adverse effects of
intuba-tion on ICP are blunted by prior administration of propofol, 1.5–3.0
mg/kg, and a rapid-onset NMB. Succinylcholine may produce mild and transient
increases in ICP in patients with closed head injury;
however, the necessity
for expeditious airway man-agement trumps these concerns. Rocuronium is often
used to facilitate intubation. Video laryngos-copy performed with in-line
stabilization generally permits neutral position intubation of the trauma
patient. An intubating bougie should be available to facilitate tube placement.
If a difficult intubation is encountered with video laryngoscopy, fiberoptic or
other techniques (eg, intubating LMA) can be attempted. If airway attempts are
unsuccessful, a surgical airway should be obtained. Blind nasal intu-bation is
contraindicated in the presence of a basilar skull fracture, which is suggested
by CSF rhinorrhea or otorrhea, hemotympanum, or ecchymosis into periorbital
tissues (raccoon sign) or behind the ear (Battle’s sign).
Hypotension
Hypotension in the setting of head trauma is nearly always
related to other associated injuries (often intraabdominal). Bleeding from
scalp lacerations may be responsible in children. Hypotension may be seen with
spinal cord injuries because of
the sympathectomy associated with spinal shock. In a patient with head trauma,
correction ofhypotension and control of any bleeding take pre-cedence over
radiographic studies and definitive neurosurgical treatment because systolic
arterial blood pressures of less than 80 mm Hg predict a poor outcome.
Glucose-containing or hypotonic solutions should not be used (see above).
Other-wise, a mix of colloid, crystalloid, and blood prod-ucts can be
administered as necessary. Massive blood loss in the patient with multiple
injuries should result in activation of a massive transfusion protocol to
provide a steady supply of platelets, fresh frozen plasma, and packed red blood
cells. Invasive monitoring of arterial pressure, central venous pressure, and
ICP are valuable, but should not delay diagnosis and treatment. Arrhythmias and
electrocardiographic abnormalities in the T wave, U wave, ST segment, and QT
interval are common following head injuries, but are not neces-sarily
associated with cardiac injury; they likely represent altered autonomic
function.
Diagnostic Studies
The choice between operative and medical
manage-ment of head trauma is based on radiographic and clinical findings.
Patients should be stabilized prior to any CT or other imaging studies.
Critically ill patients should be closely monitored during such studies.
Restless or uncooperative patients may additionally require general anesthesia.
Sedation without control of the airway should generally be avoided because of
the risk of further increases in ICP from hypercapnia or hypoxemia.
INTRAOPERATIVE MANAGEMENT
Anesthetic management is generally similar to that for other
mass lesions associated with intracranial hypertension. Management of the
airway is dis-cussed above. Invasive monitoring should be estab-lished, if not
already present, but should not delay surgical decompression in a rapidly
deteriorating patient.
Anesthetic technique and agents are
designed to preserve cerebral perfusion and mitigate increases in intracranial
pressure. Hypotension may occur after induction of anesthesia as a result of
the combined effects of vasodilation and hypovolemia and should be treated with
an α-adrenergic agonist and volume infusion if necessary.
Subsequent hypertension is common with surgical stimulation, but may also occur
with acute elevations in ICP. The latter may be associated with bradycardia
(Cushing reflex).
Hypertension can be treated with
additional doses of the induction agent, with increased concen-trations of an
inhalation anesthetic or vasodilators. β-Adrenergic blockade is usually
effective in con-trolling hypertension associated with tachycardia. CPP should
be maintained between 70 and 110 mm Hg. Vasodilators should be avoided until
the durais opened. Hyperventilation to a Paco2<30
should be avoided in trauma patients to avoid excessive decreases in oxygen
delivery.
Disseminated intravascular coagulation
occa-sionally may be seen with severe head injuries. Such injuries cause the
release of large amounts of brain thromboplastin and may also be associated
with the acute respiratory distress syndrome. Pulmonary aspiration and
neurogenic pulmonary edema may also be responsible for deteriorating lung
function. PEEP can be applied on the ventilator. When PEEP is used, ICP
monitoring can be useful to confirm an adequate CPP. Diabetes insipidus,
characterized by excessive dilute urine, is frequently seen following injuries
to the pituitary stalk. Other likely causes of polyuria should be excluded and
the diagnosis con-firmed by measurement of urine and serum osmo-lality prior to
treatment with fluid restriction and vasopressin Gastrointestinal bleeding is
common in patients not receiving prophylaxis; it is usually due to stress
ulceration.
The decision whether to extubate the
trachea at the conclusion of the surgical procedure depends on the severity of
the injury, the presence of concomi-tant abdominal or thoracic injuries,
preexisting ill-nesses, and the preoperative level of consciousness. Young
patients who were conscious preoperatively may be extubated following the
removal of a local-ized lesion, whereas patients with diffuse brain injury
should remain intubated. Moreover, persis-tent intracranial hypertension
requires continued paralysis, sedation, and hyperventilation.
Related Topics