Chapter: Clinical Anesthesiology: Anesthetic Management: Anesthesia for Patients with Liver Disease
Anesthesia for Coagulation in Liver Disease
COAGULATION IN LIVER DISEASE
In stable chronic liver disease, the causes
of exces-sive bleeding primarily involve severe thrombocyto-penia, endothelial
dysfunction, portal hypertension, renal failure, and sepsis. However, the
hemostatic changes that occur with liver disease may cause hypercoagulation and
thrombosis, as well as an increased risk of bleeding. Clot breakdown may be
enhanced by an imbalance of the fibrinolytic system.
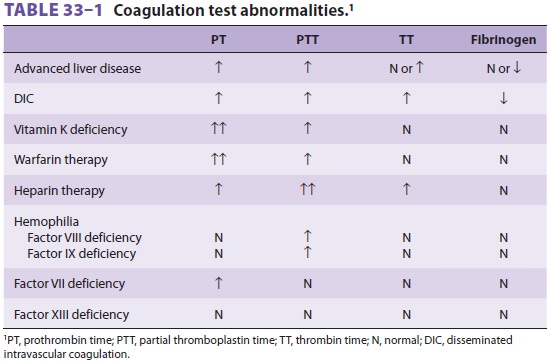
Chronic liver disease is characterized by the impaired synthesis of
coagulation factors, resulting in prolongation of the prothrombin time (PT) and
international normalized ratio (INR) (Table 33–1).
However, the anticoagulant factors (protein C, anti-thrombin, and tissue factor
pathway inhibitor) are also reduced and may balance out any effect of a
prolonged PT. This may be confirmed by assessing thrombin generation in the
presence of endothelial-produced thrombomodulin. Adequate thrombin production
requires an adequate number of functioning platelets. If the platelet count is >60,000/μL, coagulation may well be normal in a patient with severe cirrhosis.
The patient with cirrhosis will typically have hyperfibrinolysis.
However, there is a delicate bal-ance between the activators and inactivators
that regulate the conversion of plasminogen to plasmin, and, therefore,
individual laboratory tests may not give a true picture of the state of
fibrinolysis. The thromboelastography (TEG ®), rotational
thrombo-elastometry (ROTEM®), and Sonoclot®
technolo-gies are the optimal methods of demonstrating the global state of the
coagulation system at a specific moment in time in any patient with liver
disease.
Related Topics