Chapter: Clinical Anesthesiology: Anesthetic Management: Anesthesia for Patients with Liver Disease
Anesthesia for Acute Hepatitis
ACUTE HEPATITIS
Acute hepatitis is usually the result of a
viral infec-tion, drug reaction, or exposure to a hepatotoxin. The illness
represents acute hepatocellular injury with a variable degree of cellular
necrosis. Clinical manifestations depend both on the severity of the
inflammatory reaction, and, more importantly, on the degree of necrosis. Mild
inflammatory reactions may present merely as asymptomatic elevations in the
serum transaminases, whereas massive hepatic necrosis presents as acute
fulminant hepatic failure.
Viral Hepatitis
Viral hepatitis is most commonly due to hepa-titis A, hepatitis B, or
hepatitis C viral infection. At least two other hepatitis viruses have also
been identified: hepatitis D (delta virus) and hepa-titis E (enteric non-A,
non-B). Hepatitis types and E are transmitted by the fecal-oral route, whereas
hepatitis types B and C are transmitted primarily percutaneously and by contact
with body fluids. Hepatitis D is unique in that it may be transmitted by either
route and requires the pres-ence of hepatitis B virus in the host to be
infective. Other viruses may also cause hepatitis, including Epstein–Barr,
herpes simplex, cytomegalovirus, and coxsackieviruses.
Patients with viral hepatitis often have a 1-
to 2-week mild prodromal illness (fatigue, malaise, low-grade fever, or nausea
and vomiting) that may or may not be followed by jaundice. The jaundice
typically lasts 2–12 weeks, but complete recovery, as evidenced by serum
transaminase measurements, usually takes 4 months. Because clinical
manifes-tations overlap, serological testing is necessary to determine the causative
viral agent. The clinical course tends to be more complicated and prolonged
with hepatitis B and C viruses relative to other types of viral hepatitis.
Cholestasis may be a major
manifestation. Rarely, fulminant hepatic fail-ure (massive hepatic necrosis)
can develop.
The incidence of chronic active
hepatitis is 3% to 10% following
infection with hepati-tis B virus and at least 50% following infection with
hepatitis C virus. A small percentage of patients (mainly immunosuppressed
patients and those on long-term hemodialysis regimens) become asymp-tomatic
infectious carriers following infection with hepatitis B virus, and up to 30%
of these patients remain infectious with the hepatitis B surface anti-gen
(HBsAg) persisting in their blood. Most patients with chronic hepatitis C
infection seem to have very low, intermittent, or absent circulating viral
particles and are therefore not highly infective. Approximately 0.5% to 1% of
patients with hepatitis C infection become asymptomatic infectious car-riers,
and infectivity correlates with the detection of hepatitis C viral RNA in
peripheral blood. Such infectious carriers pose a major health hazard to
operating room personnel.
In addition to “universal precautions” for
avoiding direct contact with blood and secretions (gloves, mask, protective
eyewear, and not recapping needles), immunization of healthcare personnel is
highly effective against hepatitis B infection. A vac-cine for hepatitis C is
not available; moreover, unlike hepatitis B infection, hepatitis C infection
does not seem to confer immunity to subsequent exposure. Postexposure
prophylaxis with hyperimmune glob-ulin is effective for hepatitis B, but not
hepatitis C.
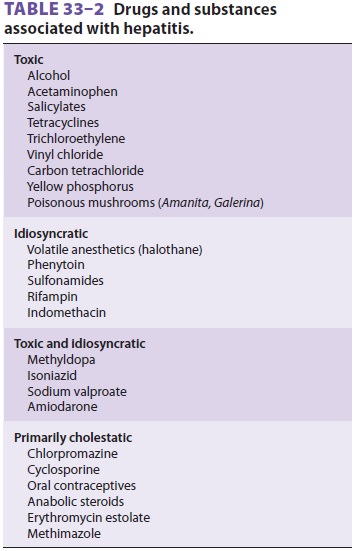
Drug-induced Hepatitis
Drug-induced hepatitis (Table 33–2) can result from direct, dose-dependent toxicity of a drug or drug
metabolite, an idiosyncratic drug reaction, or a combination of these two
causes. The clinical course often resembles viral hepatitis, making diagnosis
difficult. Alcoholic hepatitis is probably the most common form of drug-induced
hepatitis, but the etiology may not be obvious from the history. Chronic
alcohol ingestion can also result in hepato-megaly from fatty infiltration of
the liver, which reflects impaired fatty acid oxidation, increased uptake and esterification
of fatty acids, and diminished lipoprotein synthesis and secretion.
Acetaminophen ingestion of 25 g or more usually results in fatal fulminant
hepatotoxicity. A few drugs, such as chlorpromazine and oral contracep-tives,
may cause cholestatic-type reactions . Ingestion of potent hepatotoxins, such
as carbon tetrachloride and certain species of
mushrooms (Amanita, Galerina),
also may result in fatal hepatotoxicity.
Because of the increased risk of perioperative
morbidity and mortality, patients with acute hepatitis should have elective
surgery postponed until the illness has resolved, as indicated by the
nor-malization of liver tests. In addition, acute alcohol toxicity greatly
complicates anesthetic management, and acute alcohol withdrawal during the
periopera-tive period may be associated with a mortality rate as high as 50%.
Only emergent surgery should be considered for patients presenting in acute
alcohol withdrawal. Patients with hepatitis are at risk of deterioration of
hepatic function and the develop-ment of complications from hepatic failure,
such as encephalopathy, coagulopathy, or hepatorenal syndrome.
Laboratory evaluation of the patient with
hep-atitis should include blood urea nitrogen, serum electrolytes, creatinine,
glucose, transaminases, bili-rubin, alkaline phosphatase, and albumin, platelet
count, and PT. Serum should also be checked for HBsAg whenever possible. A
blood alcohol level is useful if the history or physical examination is compatible
with ethanol intoxication. Hypokalemia and metabolic alkalosis are not uncommon
and are usually due to vomiting. Concomitant hypo-magnesemia may be present in
chronic alcoholics and predisposes to cardiac arrhythmias. The eleva-tion in
serum transaminases does not necessarily correlate with the amount of hepatic
necrosis. The serum alanine aminotransferase (ALT) is generally higher than the
serum aspartate aminotransfer-ase (AST), except in alcoholic hepatitis, where
the reverse occurs. Bilirubin and alkaline phosphatase are usually only
moderately elevated, except with the cholestatic variant of hepatitis. The PT
is the best indicator of hepatic synthetic function. Persistent prolongation of
longer than 3 sec (INR > 1.5) fol-lowing administration of vitamin K is indicative of severe
hepatic dysfunction. Hypoglycemia is not uncommon. Hypoalbuminemia is usually
not pres-ent except in protracted cases, with severe malnutri-tion, or when
chronic liver disease is present.
If a patient with acute hepatitis must undergo an emergent operation,
the preanesthetic evalua-tion should focus on determining the cause and the
degree of hepatic impairment. Information should be obtained regarding recent
drug exposures, including alcohol intake, intravenous drug use, recent
transfusions, and prior anesthetics. The pres-ence of nausea or vomiting should
be noted, and, if present, dehydration and electrolyte abnormalities should be
anticipated and corrected. Changes in mental status may indicate severe hepatic
impair-ment. Inappropriate behavior or obtundation in alcoholic patients may be
signs of acute intoxica-tion, whereas tremulousness and irritability usually
reflect withdrawal. Hypertension and tachycardia are often also prominent with
the latter. Fresh fro-zen plasma may be necessary to correct a coagu-lopathy.
Premedication is generally not given, in an effort to minimize drug exposure
and not confound hepatic encephalopathy in patients with advanced liver
disease. However, benzodiazepines and thia-mine are indicated in alcoholic
patients with, or at risk for, acute withdrawal.
Intraoperative Considerations
The goal of intraoperative management is to
preserve existing hepatic function and avoid factors that may be detrimental to
the liver. Drug selection and dos-age should be individualized. Some patients
with viral hepatitis may exhibit increased central ner-vous system sensitivity
to anesthetics, whereas alco-holic patients will often display cross-tolerance
to both intravenous and volatile anesthetics. Alcoholic patients also require
close cardiovascular monitoring, because the cardiac depressant effects of
alcohol are additive to those of anesthetics; moreover, alcoholic
cardiomyopathy is present in many alcoholic patients.
Inhalation anesthetics are generally
preferable to intravenous agents because most of the latter are dependent on
the liver for metabolism or elimina-tion. Standard induction doses of
intravenous induction agents can generally be used because their action is terminated
by redistribution rather than metabolism or excretion. A prolonged duration of
action, however, may be encountered with large or repeated doses of intravenous
agents, particularlyopioids. Isoflurane and sevoflurane are the volatile agents
of choice because they preservehepatic blood flow and oxygen delivery. Factors
known to reduce hepatic blood flow, such as hypo-tension, excessive sympathetic
activation, and high mean airway pressures during controlled ventila-tion,
should be avoided. Regional anesthesia, includ-ing major conduction blockade,
may be employed in the absence of coagulopathy, provided hypotension is
avoided.
Related Topics