Chapter: Clinical Anesthesiology: Anesthetic Management: Anesthesia for Patients with Respiratory Disease
Anesthesia : Pulmonary Risk Factors
PULMONARY RISK FACTORS
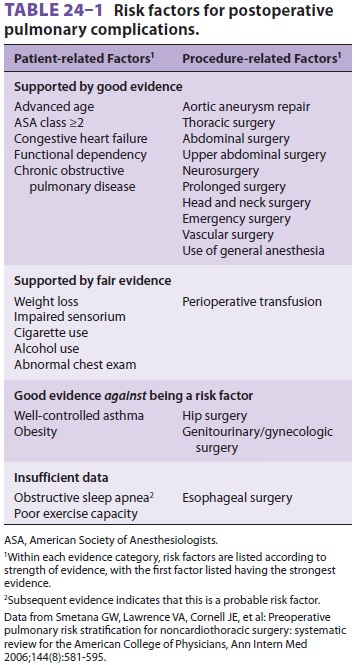
Certain risk factors (Table 24–1) may
predispose patients to postoperative pulmonary complica-tions. The incidence of
atelectasis, pneumonia,pulmonary embolism, and respiratory failure fol-lowing
surgery is quite high, but varies widely (from 6% to 60%), depending on the
patient population studied and the surgical procedures performed. The two
strongest predictors of complications seem to be operative site and a history of
dyspnea, which correlate with the degree of preexisting pulmonary disease.
The association between smoking and
respi-ratory disease is well established; abnormalities in maximal
midexpiratory flow (MMEF) rates are often demonstrable well before symptoms of
COPD appear. Although abnormalities can be demon-strated on pulmonary function
tests (PFTs), because most patients who smoke do not have PFTs per-formed
preoperatively, it is best to assume that such patients have some degree of
pulmonary compro-mise. Even in normal individuals, advancing age is associated
with an increasing prevalence of pul-monary disease and an increase in closing
capac-ity. Obesity decreases functional residual capacity (FRC), increases the
work of breathing, and predis-poses patients to deep venous thrombosis.
Thoracic and upper abdominal surgical proce-dures can have marked effects on pulmonary func-tion. Operations near the diaphragm often result in diaphragmatic dysfunction and a restrictive ventilatory defect . Upper abdominal procedures consistently decrease FRC (60% to 70%); the effect is maximal on the first postoperative day and usually lasts 7–10 days. Rapid shallow breathing with an ineffective cough caused by pain (splinting), a decrease in the number of sighs, and impaired mucociliary clearance lead to microatelectasis and loss of lung volume. Intrapulmonary shunting pro-motes hypoxemia. Residual anesthetic effects, the recumbent position, sedation from opioids, abdomi-nal distention, and restrictive dressings may also be contributory. Complete relief of pain with regional
anesthesia can decrease, but does not
completely reverse these abnormalities. Persistent microatelec-tasis and
retention of secretions favor the develop-ment of postoperative pneumonia.
Although many adverse effects of general
anes-thesia on pulmonary function have been described, the superiority of
regional over general anesthesia in patients with pulmonary impairment is not
firmly established.
Because of the prevalence of smoking and
obe-sity, many patients may be at increased risk of devel-oping postoperative
pulmonary dysfunction. The risk of complications increases if the patient is
hav-ing a thoracotomy or laparotomy, even if the patient has no risk factors.
Patients with known disease should have their pulmonary function optimized
preoperatively, with careful consideration given to the choice of general
versus regional anesthesia.
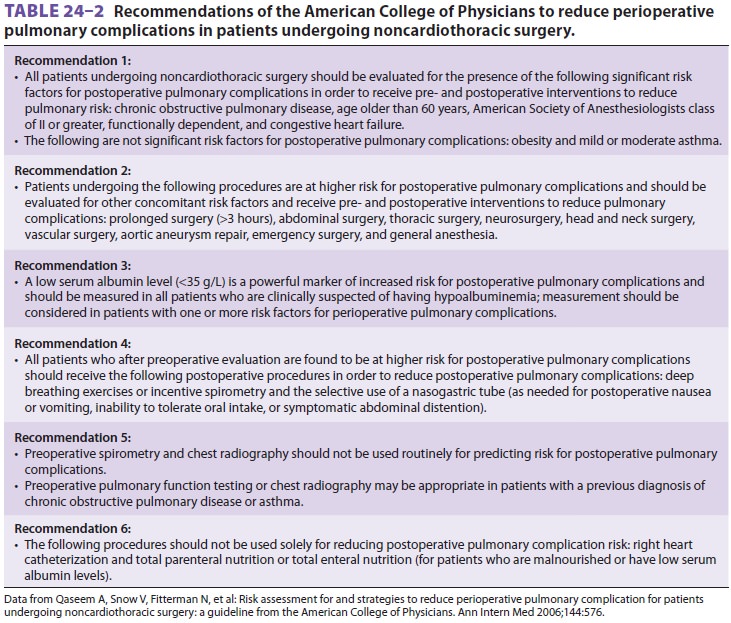
The American College of Physicians has
estab-lished guidelines to assist in the preoperative assess-ment of patients
with pulmonary disease (see Table 24–2).
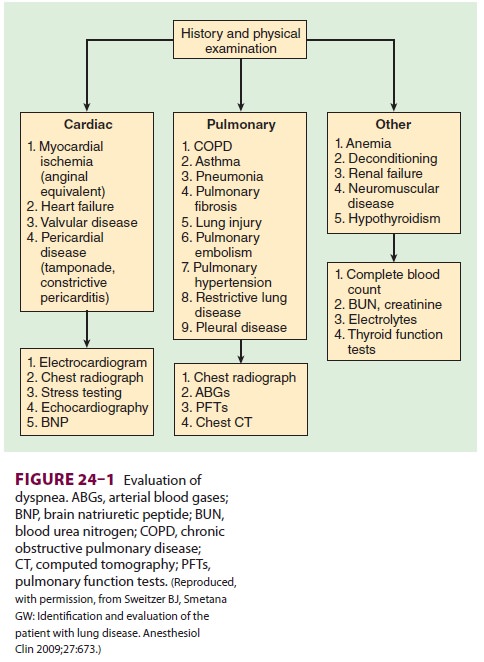
When patients with a history of dyspnea
present without the benefit of a previous workup, the differ-ential diagnosis
can be quite broad and may include both primary pulmonary and cardiac
pathologies. Diagnostic approaches to evaluating such patients are summarized
in Figure24–1.
Obstructive Pulmonary Disease
Obstructive
and restrictive breathing are the two most common abnormal patterns, as
determined by PFTs. Obstructive lung diseases are the most com-mon form of
pulmonary dysfunction. They include asthma, emphysema, chronic bronchitis,
cystic fibrosis, bronchiectasis, and bronchiolitis. The pri-mary characteristic
of these disorders is resistance to airflow. An MMEF of <70% (forced
expiratory flow [FEF25–75%]) is often the only abnormality early in
the course of these disorders. Values for FEF25–75% in adult males
and females are normally >2.0
and >1.6
L/sec, respectively. As the disease progresses, both forced expiratory volume
in 1 sec (FEV1) and the FEV1/FVC (forced vital capacity)
ratio are less than 70% of the predicted values.
Elevated
airway resistance and air trap-ping increase the work of breathing; respiratory
gas exchange· is·
impaired because of ventilation/ perfusion (V/Q) imbalance. The predominance of
expiratory airflow resistance results in air trap-ping; residual volume and
total lung capacity (TLC) increase. Wheezing is a common finding and
repre-sents turbulent airflow. It is often absent with mild obstruction that
may be manifested initially only by prolonged exhalation. Progressive
obstruction typi-cally results first in expiratory wheezing only, and then in
both inspiratory and expiratory wheezing. With marked obstruction, wheezing may
be absent when airflow has nearly ceased.
Related Topics