Chapter: Basic & Clinical Pharmacology : Introduction to Autonomic Pharmacology
Anatomy of the Autonomic Nervous System
ANATOMY OF THE AUTONOMIC NERVOUS
SYSTEM
The
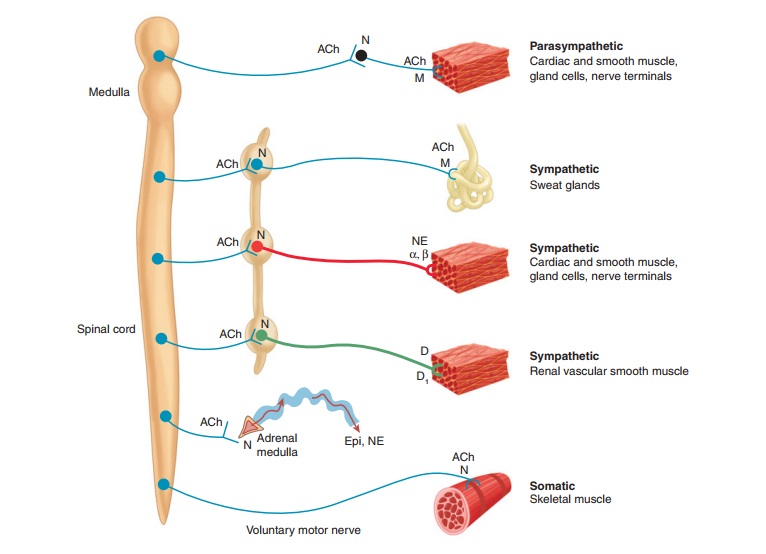
ANS lends itself to division on anatomic grounds into two major portions: the sympathetic (thoracolumbar) division
and the parasympathetic (craniosacral) division
(Figure 6–1). Neurons inboth divisions originate in nuclei within the CNS and
give rise to preganglionic efferent fibers that exit from the brain stem or
spinal cord and terminate in motor ganglia. The sympathetic preganglionicfibers
leave the CNS through the thoracic and lumbar spinal nerves. The
parasympathetic preganglionic fibers leave the CNS through the cranial nerves
(especially the third, seventh, ninth, and tenth) and the third and fourth
sacral spinal nerve roots.
Most
sympathetic preganglionic fibers are short and terminate in ganglia located in
the paravertebral chains that lie on
either side of the spinal column. The remaining sympathetic preganglionic
fibers are somewhat longer and terminate in prevertebral ganglia, which lie in front of the vertebrae, usually
on the ventral surface of the aorta. From the ganglia, postganglionic
sympathetic fibers run to the tissues innervated. Some preganglionic
parasympathetic fibers terminate in parasympathetic ganglia located outside the
organs innervated: the ciliary,
pterygopalatine, submandibular,otic, and several pelvic ganglia. However, the majority of para-sympathetic
preganglionic fibers terminate on ganglion cells dis-tributed diffusely or in
networks in the walls of the innervatedorgans. Note that the terms
“sympathetic” and “parasympathetic” are anatomic designations and do not depend
on the type of trans-mitter chemical released from the nerve endings nor on the
kind of effect—excitatory or inhibitory—evoked by nerve activity.
In
addition to these clearly defined peripheral motor portions of the ANS, large
numbers of afferent fibers run from the periph-ery to integrating centers,
including the enteric plexuses in the gut, the autonomic ganglia, and the CNS.
Many of the sensory pathways that end in the CNS terminate in the integrating
centers of the hypothalamus and medulla and evoke reflex motor activity that is
carried to the effector cells by the efferent fibers described previously.
There is increasing evidence that some of these sensory fibers also have
peripheral motor functions.
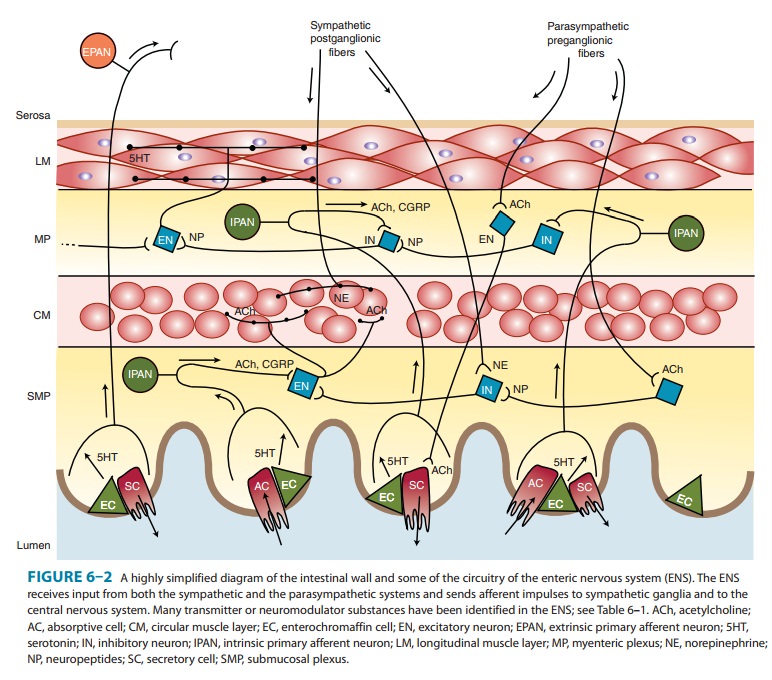
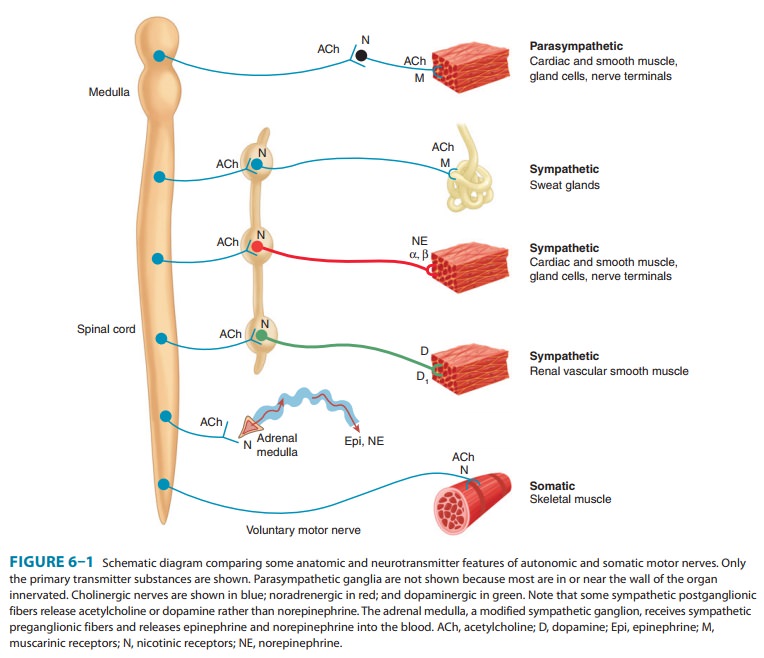
The
enteric nervous system (ENS) is a
large and highly orga-nized collection of neurons located in the walls of the
gastrointes-tinal (GI) system (Figure 6–2). It is sometimes considered a third
division of the ANS. It is found in the wall of the GI tract from the esophagus
to the distal colon and is involved in both motor and secretory activities of
the gut. It is particularly critical in the motor activity of the colon. The
ENS includes the myenteric plexus
(the plexus of Auerbach) and the submucous
plexus (the plexus of Meissner). These neuronal networks receive
preganglionic fibers from the parasympathetic system and postganglionic
sympathetic axons. They also receive sensory input from within the wall of the
gut. Fibers from the neuronal cell bodies in these plexuses travel forward,
backward, and in a circular direction to the smooth muscle of the gut to control
motility and to secretory cells in the mucosa. Sensory fibers transmit chemical
and mechanical informa-tion from the mucosa and from stretch receptors to motor
neurons in the plexuses and to postganglionic neurons in the sympathetic
ganglia. The parasympathetic and sympathetic fibers that synapse on enteric
plexus neurons appear to play a modulatory role, as indicated by the
observation that deprivation of input from both ANS divisions does not abolish
GI activity. In fact, selective dener-vation may result in greatly enhanced
motor activity.
The
ENS functions in a semiautonomous manner, utilizing input from the motor
outflow of the ANS for modulation of GI activity and sending sensory
information back to the CNS. The ENS also provides the necessary synchronization
of impulses that, for example, ensures forward, not backward, propulsion of gut
contents and relaxation of sphincters when the gut wall contracts.
The
anatomy of autonomic synapses and junctions determines the localization of
transmitter effects around nerve endings. Classic synapses such as the
mammalian neuromuscular junction and most neuron-neuron synapses are relatively
“tight” in that the nerve terminates in small boutons very close to the tissue
inner-vated, so that the diffusion path from nerve terminal to postsyn-aptic
receptors is very short. The effects are thus relatively rapid and localized.
In contrast, junctions between autonomic neuron terminals and effector cells
(smooth muscle, cardiac muscle, glands) differ from classic synapses in that
transmitter is often released from a chain of varicosities in the
postganglionic nerve fiber in the region of the smooth muscle cells rather than
from boutons, and autonomic junctional clefts are wider than somatic synaptic
clefts. Effects are thus slower in onset and discharge of a single motor fiber
often activates or inhibits many effector cells.
Related Topics