Chapter: Modern Medical Toxicology: Corrosive(Caustic) Poisons: Alkalis and Other Caustics
Alkalis - Corrosive(Caustic) Poisons
Alkalis
and Other Caustics
ALKALIS
Alkalis
commonly encountered in poisoning include ammonia (usually in the form of
ammonium hydroxide), carbonates of sodium and potassium, and hydroxides of
sodium, potassium, and calcium. Sodium hypochlorite is also increasingly being
implicated.
Physical Appearance
Most of these occur as white powders
or colourless solutions. Ammonia gas is colourless with a pungent, choking
odour.
Uses
·
Ammonia
gas—Smelling salts.*
·
Ammonium
hydroxide (32.5% ammonia)—Paint,
oil, and dirt remover, refrigerant.
·
Sodium
hydroxide (caustic soda)—Drain
cleaner, oven cleaner. Potassium
hydroxide (caustic potash)—Drain
cleaner, hearing aid batteries.
·
Sodium
carbonate (washing soda)—Household
cleaning agent, detergent.
·
Potassium
carbonate—Household cleaning agent.
·
Sodium
hypochlorite—Household bleach.
Usual Fatal Dose
·
About 10 to 15 gm for most alkalis.
·
About 15 to 20 ml for ammonia.
Mode of Action
Locally,
alkalis produce liquefaction necrosis which results in extensive penetrating
damage because of saponification of fats and solubilisation of proteins.
Production of ulcers is common which may persist for several weeks. Oesophagus
is more severely affected than the stomach in contrast to acids.
Clinical Features
Corrosion of GI mucosa with greyish
pseudomembrane formation. Oesophagus is often severely affected resulting in
dysphagia, vomiting, drooling, and haematemesis. Stridor is an important
indicator of severe oesophageal injury.
There
are four categories of alkali induced oesophagitis:
a. Non-ulcerative oesophagitis—from
ingestion of mildirritants, resulting in 1st degree burns.
b.Mild ulcerative oesophagitis—from
ingestion of weakbases. 2nd degree burns are produced. Strictures may develop.
c.Severe ulcerative oesophagitis—from
ingestion ofstrong bases. There is severe dysphagia with vomiting which may
subside after 2 to 3 days only to reappear as slowly progressive dysphagia
after 4 to 6 weeks due to stricture formation. This may lead to total
obstruction.
d.Oesophagitis with complications—apart
fromoesophagitis, there are complications such as medi-astinitis, perforation,
pericarditis, pulmonary oedema, laryngeal obstruction, etc.
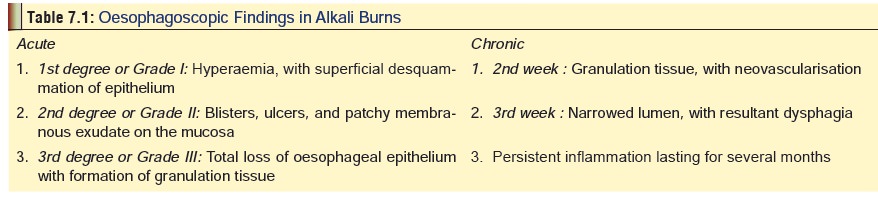
It
is important to perform oesophagoscopy and make accurate assessment as to the
extent of local injury (Table 7.1).
Contraindications to oesophagoscopy include upper airway obstruction and GI
perforation.
Abdominal
pain, diarrhoea, tenesmus. Skin involvement results in greyish, soapy, necrotic
areas without charring.
Eye
involvement can produce serious complications, and constitutes an
ophthalmologic emergency.
Ammonia
ingestion causes manifestations which are essen-tially similar to those seen
with other alkalis, but respiratory symptoms are commonly super-added due to
inhalation of fumes while swallowing.
Diagnosis
1.In stomach contents:
a. White, solid, slimy lumps,
flakes, or granules.
b.Turns litmus paper blue.
c.Becomes warm on addition of water.
d.If exposed to air, becomes moist
and gets dissolved.
e.Soapy or slimy feeling when
touched with fingers.
f.Sharp penetrating odour in the
case of ammonia.
2.Platinum wire flame test: Touch platinum wire to theunknown
substance and then place it in a flame. Sodium gives an intense persistent
yellow flame. Potassium gives a deep purple flame.
3.Fume test for ammonia: Place an open bottle of
concen-trate Hcl near a sample of stomach contents, aspirate, or vomitus.
Copious white fumes of ammonium chloride will emanate if ammonia is present.
The test can also be done to detect the presence of ammonia in the atmosphere.
Treatment
·
Respiratory distress (especially in the case of ammonia) may
require endotracheal intubation, cricothyroidotomy, or tracheostomy, depending
on severity. Oxygen must be administered as necessary.
·
Diluents such as milk or water may be given as a first aid
measure for alkali ingestion (no more than one or two glasses for an adult). If
more than one hour has elapsed, this is usually not efficacious.
·
The following are absolutely contraindicated : emesis,gastric
lavage, catharsis, and activated
charcoal. Withhold all oral feeds initially.
·
Assess fluid and electrolyte balance.
·
Watch for development of complications and attend to them
accordingly.
·
Some investigators recommend early surgical intervention and
use of an intraluminal stent in patients with 2nd or 3rd degree oesophageal
burns because perforation which requires surgical repair may otherwise be
missed. Others have suggested that if the serum pH is less than 7.20 (because
of lactic acidosis resulting from severe tissue necrosis), surgery should be
immediately undertaken.
·
If circumferential 2nd degree or 3rd degree burns of the
oesophagus are seen, exploratory laparotomy should be undertaken followed by
gastric resection and oesopha-gectomy, in case gastric necrosis is evident at
laparos-copy.
·
In the past, administration of corticosteroids was recom-mended
to prevent stricture formation which was based on animal studies. But today
most investigators appear to be of the opinion that high dose corticosteroid
therapy in caustic ingestion predisposes the patient to infection and
perforation as well as masks symptoms of devel-oping peritonitis or
mediastinitis, and hence should be avoided. However, steroids may be effective
in patients with dyspnoea, stridor, hoarseness, and other evidence of
respiratory compromise, and may decrease laryngotra-cheal oedema thereby
lessening respiratory dysfunction.
·
Use of prophylactic antibiotics is not recommended today.
Most investigators feel that antibiotics should be administered only if there
are signs of perforation or secondary infection.
·
An oesophagogram should be done at 3 weeks to evaluate the
formation of strictures. Patients should be instructed to seek medical
attention immediately when-ever they develop dysphagia.
·
Alkali injuries to the eye and skin should be irrigated
copiously with water or saline for at least 20 to 30 minutes. Ophthalmologic
consultation is mandatory. Topical antibiotics and steroids may help.
·
Patients who have suffered from stricture formation require
long-term endoscopic follow-up for the presence of neoplastic changes of the
oesophagus which may occur with a delay of several years or decades.
Autopsy Features
· Characteristic odour (in the case of
ammonia).
· Brownish or greyish staining of
skin.
· Inflammatory oedema with corrosion
and sliminess of the tissues of the oesophagus and stomach. The mucosa may be
brownish owing to formation of alkaline haematin.
·
Congestion of respiratory tract and pulmonary oedema
(especially in the case of ammonia).
Forensic Issues
·
Accidental poisoning occurs usually
by mistaking an alkali solution for water, lemonade, beer, etc., because of
careless storage of these chemicals in inadequately labeled, ordinary looking
bottles or jars.
·
Industrial accidents involving these
substances are reported from time to time.
·
Suicidal cases are occasionally
encountered. Homicides from time to time.
·
Suicidal cases are occasionally
encountered. Homicides are quite rare.
·
Ammonia may sometimes be sprayed or
thrown on a victim to facilitate robbery.
Related Topics