Chapter: Clinical Cases in Anesthesia : Spinal Anesthesia
What factors affect the spread of anesthetic within the subarachnoid space?
What factors affect the spread of anesthetic within the
subarachnoid space?
Specific gravity greatly influences the local
anesthetic’s spread within the subarachnoid space. The specific gravity of CSF
ranges between 1.003 and 1.008. Local anesthetics with lower specific
gravities, i.e., hypobaric solutions, tend to float toward the nondependent
areas. Hypobaric solutions have been used for patients with fractured hips,
placing the injured extremity above as the patient lies in the lateral
decubitus position. Hypobaric solutions are created by dis-solving local
anesthetic in distilled water. Local anesthetic solutions with specific
gravities above 1.008 are hyperbaric. Hyperbaric solutions tend to migrate
toward dependent areas. They are the local anesthetic preparations most
commonly used for spinal anesthesia in the United States. Hyperbaric solutions
are readily adaptable to most spinal anesthetic needs and are particularly
valuable for anes-thetizing lower thoracic nerve roots and for “selectively”
anesthetizing sacral nerve roots (saddle blocks). Hyperbaric solutions are created
by mixing a local anesthetic with 10% dextrose in water. Level of the dural
puncture and patient position also affect anesthetic spread.
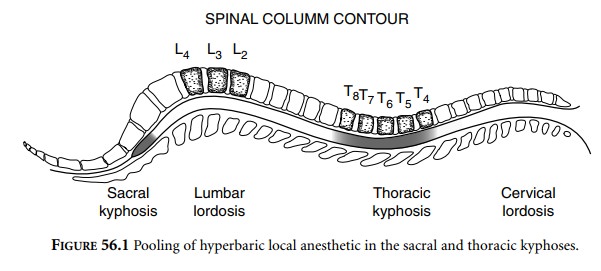
The spinal column contains a natural lumbar
lordosis as well as a thoracic and sacral kyphosis. L4 resides at
the peak of the lumbar lordosis, and T5 lies at the nadir of the
thoracic kyphosis (Fig. 56.1). After local anesthetic is injected at the L4
level and the patient is turned to the supine posi-tion, hyperbaric solutions
tend to pool in the sacral and thoracic kyphoses. In other words, hyperbaric
solutions run downhill, providing maximal anesthesia of the sacral and
midthoracic nerve roots. Middle lumbar spinal roots may be exposed to minimal
amounts of local anesthetic, thereby providing poor sensory block to these
dermatomes whenever inadequate local anesthetic is administered. Raising the
legs into the lithotomy position will flatten the lumbar lordosis and help
prevent large unanesthetized windows. Pooling of solution in the thoracic
kyphosis tends to prevent anesthesia rising above the T4 dermatome,
preventing a “total spinal”. Using excessively large volumes of anesthetic may
overcome the lumbar lordosis problem but it may also spread the anesthetic
above T4. To avoid both excessively high levels and inadequate
levels, the process of selecting the proper dose of local anesthetic for
subarachnoid injection has, in the past, taken into account innumerable
variables. Height, weight, age, increased abdominal pressure, position, site of
injection, volume of injectate, concentration of local anesthetic, amount of
local anesthetic, and baricity represent only some of the factors that were
traditionally thought to significantly affect anesthetic spread. With these
criteria in mind, a myriad of guidelines for spinal anesthesia dosing have been
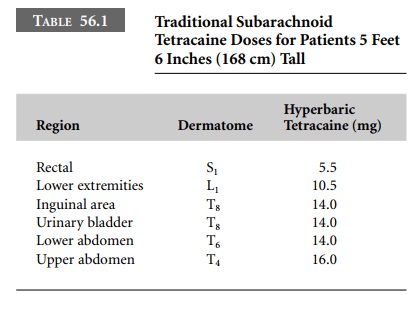
presented over the years. Table 56.1 lists one of the many possible dosing
schedules for hyperbaric tetracaine spinal anesthet-ics. It has generally been
recommended to reduce amounts by 2 mg for patients 5 feet (152 cm) tall and to increase
amounts by 2 mg for patients 6 feet (183 cm) tall. Despite rigorous adherence
to such dosing schedules, spinal anes-thesia has frequently been inadequate to
provide satisfac-tory patient comfort during surgery.
Recognizing the high frequency of
inappropriately low anesthesia levels, Norris (1988) conducted a study that has
revolutionized spinal anesthesia dosing regimens. Evaluation of term
parturients receiving 12 mg of hyperbaric bupivacaine demonstrated no
correlation between the spread of anesthesia and the subject’s height, weight,
or body mass index. Although peak analgesic levels ranged from T7–C8,
most patients attained levels between T4 and T1.
Extrapolating these results to the nonpregnant patient, several authors revised
the recommended dosing schedules for subarachnoid block. Adult patients, placed
in the supine position, can receive 15 mg of hyperbaric bupiva-caine or
hyperbaric tetracaine. These solutions will eventu-ally migrate to the T5
nerve roots, producing profound and reliable anesthesia below this level. This
technique is espe-cially useful for surgery on structures innervated below T8.
The newer recommendations calling for significantly larger local anesthetic
doses provide more intense blockade for longer durations without significantly
extending the spread of anesthesia. Tuominen and colleagues (1992) have
suggested that unpredictable individual anatomic varia-tions may play an
important role in subarachnoid spread of local anesthetics.
To prevent local anesthetic spread to thoracic
levels when only lumbosacral anesthesia is required, isobaric lidocaine 2.0% or
isobaric bupivacaine 0.5% without preservatives represent an excellent choice.
Isobaric solu-tions tend to remain in the lumbosacral area into which they are
injected. These local anesthetics do not migrate significantly, providing for
maintenance of adequate anes-thetic concentrations bathing the lumbosacral
nerve roots. The benefits include more intense analgesia, greater dura-tion of
action, and reduced potential for hypotension and respiratory depression.
Speed of anesthetic injection should
approximate 0.5 mL/sec. Significantly more rapid injection rates tend to push
the anesthetic toward higher dermatome levels.
Related Topics