Chapter: Medical Physiology: Regulation of Extracellular Fluid Osmolarity and Sodium Concentration
Urea Contributes to Hyperosmotic Renal Medullary Interstitium and to a Concentrated Urine
Urea Contributes to Hyperosmotic Renal Medullary Interstitium and to a Concentrated Urine
Thus far, we have considered only the contribution of sodium chloride to the hyperosmotic renal medullary interstitium. However, urea contributes about 40 to 50 per cent of the osmolarity (500-600 mOsm/L) of the renal medullary interstitium when the kidney is forming a maximally concentrated urine. Unlike sodium chloride, urea is passively reabsorbed from the tubule. When there is water deficit and blood concen-trations of ADH are high, large amounts of urea are passively reabsorbed from the inner medullary col-lecting ducts into the interstitium.
The mechanism for reabsorption of urea into the renal medulla is as follows: As water flows up the ascending loop of Henle and into the distal and corti-cal collecting tubules, little urea is reabsorbed because these segments are impermeable to urea (see Table 28–1). In the presence of high concentrations of ADH, water is reabsorbed rapidly from the cortical col-lecting tubule and the urea concentration increases rapidly because urea is not very permeant in this part of the tubule. Then, as the tubular fluid flows into the inner medullary collecting ducts, still more water reab-sorption takes place, causing an even higher concen-tration of urea in the fluid. This high concentration of urea in the tubular fluid of the inner medullary col-lecting duct causes urea to diffuse out of the tubule into the renal interstitium. This diffusion is greatly facilitated by specific urea transporters. One of these urea transporters, UT-AI, is activated by ADH, increasing transport of urea out of the inner medullary collecting duct even more when ADH levels are ele-vated. The simultaneous movement of water and urea out of the inner medullary collecting ducts maintains a high concentration of urea in the tubular fluid and, eventually, in the urine, even though urea is being reabsorbed.
The fundamental role of urea in contributing to urine concentrating ability is evidenced by the fact that people who ingest a high-protein diet, yielding large amounts of urea as a nitrogenous “waste” product, can concentrate their urine much better than people whose protein intake and urea production are low. Malnutrition is associated with a low urea concentra-tion in the medullary interstitium and considerable impairment of urine concentrating ability.
Recirculation of Urea from Collecting Duct to Loop of Henle Contributes to Hyperosmotic Renal Medulla. A personusually excretes about 20 to 50 per cent of the filtered load of urea. In general, the rate of urea excretion is determined mainly by two factors: (1) the concentra-tion of urea in the plasma and (2) the glomerular fil-tration rate (GFR). In patients with renal disease who have large reductions of GFR, the plasma urea con-centration increases markedly, returning the filtered urea load and urea excretion rate to the normal level (equal to the rate of urea production), despite the reduced GFR.
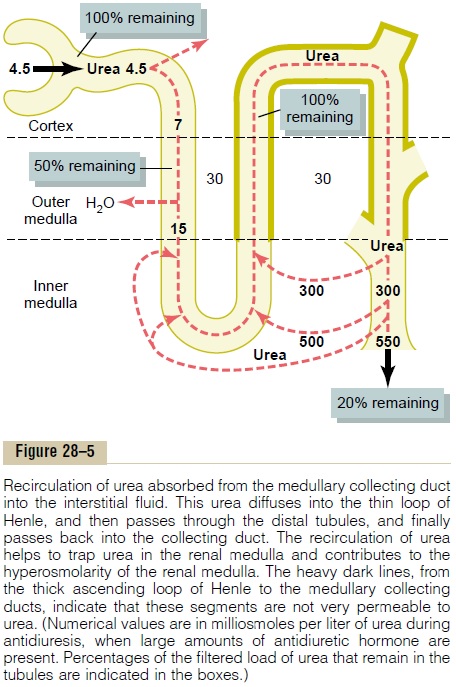
In the proximal tubule, 40 to 50 per cent of the fil-tered urea is reabsorbed, but even so, the tubular fluid urea concentration increases because urea is not nearly as permeant as water. The concentration of urea continues to rise as the tubular fluid flows into the thin segments of the loop of Henle, partly because of water reabsorption out of the descending loop of Henle but also because of some secretion of urea into the thin loop of Henle from the medullary interstitium (Figure 28–5).
The thick limb of the loop of Henle, the distal tubule, and the cortical collecting tubule are all rela-tively impermeable to urea, and very little urea reab-sorption occurs in these tubular segments. When the kidney is forming a concentrated urine and high levels of ADH are present, the reabsorption of water from the distal tubule and cortical collecting tubule further raises the tubular fluid concentration of urea. And as this urea flows into the inner medullary collecting duct, the high tubular fluid concentration of urea and specific urea transporters cause urea to diffuse into the medullary interstitium. A moderate share of the urea that moves into the medullary interstitium eventually diffuses into the thin loop of Henle, so that it passes upward through the ascending loop of Henle, the distal tubule, the cortical collecting tubule, and back down into the medullary collecting duct again. In this way, urea can recirculate through these terminal parts of the tubular system several times before it is excreted. Each time around the circuit contributes to a higher concentration of urea.
This urea recirculation provides an additional mech-anism for forming a hyperosmotic renal medulla. Because urea is one of the most abundant waste prod-ucts that must be excreted by the kidneys, this mech-anism for concentrating urea before it is excreted is essential to the economy of the body fluid when water is in short supply.
When there is excess water in the body and low levels of ADH, the inner medullary collecting ducts have a much lower permeability to both water and urea, and more urea is excreted in the urine.
Related Topics