Chapter: Obstetrics and Gynecology: Third-Trimester Bleeding
Third-Trimester Bleeding
Third-Trimester
Bleeding
Approximately 4% to 5% of
pregnancies are com
plicated by vaginal bleeding in the third trimester.
Bleeding ranges from spotting to
life-threatening hemorrhage. Intercourse and recent pelvic examinations are
common precipitants of spotting, as the cervix is more vascular and friable in
pregnancy. Twenty percent of car-diac output is shunted to the pregnant uterus,
so significant bleeding can be quickly catastrophic. Severe hemorrhage is much
less common than spotting, but remains a leading cause of maternal and fetal
morbidity and mortality. Thetwo most
common causes of significant bleeding are placenta previa (in which the
placenta is located close to or over the cervical os) and placental abruption
(premature separation of the placenta). Other important causes of bleeding
are preterm cervical change, preterm labor, and uterine rupture. In many cases,
bleeding remains unexplained or is attributed to local lesions. Possible causes
of third-trimester bleeding are listed in Box 21.1.
A focused but comprehensive
history and physical exam are crucial in assessing obstetric bleeding once the
patient is stable and a reassuring fetal heart rate pattern is confirmed. While
diagnosis is rarely based solely on his-tory, a differential diagnosis is
usually possible after perti-nent information has been gathered. It is always
important to quantify bleeding and associated symptoms, such as abdominal pain.
A personal or family history of bleeding with procedures may lead to a
diagnosis of a bleeding dis-order, whereas a history of cervical dysplasia and no
recent pap tests would be worrisome for cervical cancer. It is also important
to consider other origins of bleeding, such as hemorrhoids or bladder
disorders.
A physical examination should
always begin with vital signs. The fetal heart rate should be auscultated
either by Doppler or electronic fetal monitor. A general review of respiratory
and cardiovascular systems is warranted in all patients. Intravenous access
should be established if the bleeding is heavy, estimated blood loss is
significant, or the patient is unstable. A brief inspection for petechiae or bruising may be indicated if there is suspicion of a bleed-ing
disorder. Particular attention should be paid to the abdomen and pelvis.
Pelvic
examination should not be undertaken until placental position is confirmed, as
this could cause significant bleeding in a patient with placenta previa.
Careful inspection of the vulva
should be followed by a speculum examination of the vagina and cervix.
A common finding in pregnancy is
a significant ectro-pion of the
cervix, particularly among women with a his-tory of using oral contraceptives.
The ectropion is an area on the ectocervix where columnar epithelium has been
exposed to vaginal acidity due to eversion of the endocervix. The ectropion may
appear reddened and “raw looking.” These findings may raise concerns about
cancer, but they are actually benign.
Significant bleeding requires
immediate management, including ongoing monitoring of vital signs and two large
bore intravenous lines for administration of crystalloid fluid. Blood studies
should include complete blood count, coagulation profile, and a type and cross
match for 4 units. Regardless of the amount of bleeding, blood type and screen
are necessary. Patients who are Rh
D-negative may requireimmunoglobulin to protect against the Rh D antigen and a Kleihauer-Betke test or other test to
determine feto—maternalbleeding should be performed to determine the amount of
immunoglobulin needed once the bleeding has been controlled. Staff should
be ready for deliv-ery. Most likely, this will require an emergency caesarean
delivery and, possibly, a general anesthetic. If the bleeding is not sufficient
to warrant emergency delivery and/or the fetus is preterm, then blood studies
should be continued and intervenous access maintained. An ultrasound
examination should be performed to assess placental location and condi-tion of
the fetus. The patient should be admitted to the hos-pital to allow for close
monitoring.
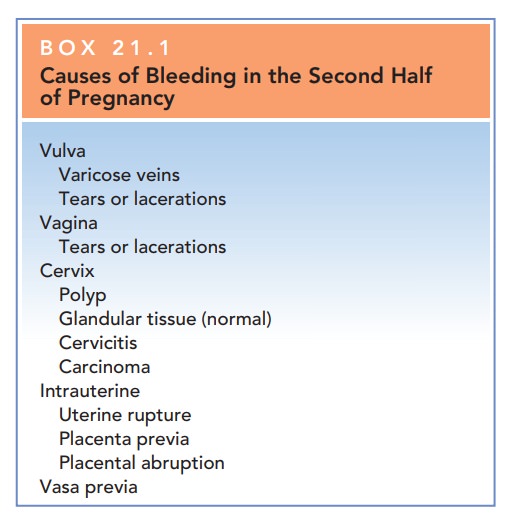
Box 21.1
Causes of Bleeding in the Second Half of Pregnancy
Vulva
·
Varicose veins
·
Tears or lacerations
Vagina
·
Tears or lacerations
Cervix
·
Polyp
·
Glandular tissue (normal)
·
Cervicitis
·
Carcinoma
Intrauterine
·
Uterine rupture
·
Placenta previa
·
Placental abruption
Vasa previa
Related Topics