Chapter: Obstetrics and Gynecology: Preterm Labor
Management of Preterm Labor
MANAGEMENT OF PRETERM LABOR
The
purpose in treating preterm labor is to delay delivery, if possible, until
fetal maturity is attained.
Management involves two broad
goals: (1) the detection and treatment of disorders associated with preterm
labor, and (2) therapy for the preterm labor itself. Fortunately,more than 50% of patients with preterm contractions have
spontaneous resolution of abnormal uterine activity. However,this
complicates the evaluation of effectiveness of specific treatments, because it
is unclear if the contractions would have resolved spontaneously or if their
cessation was due to effective treatments.
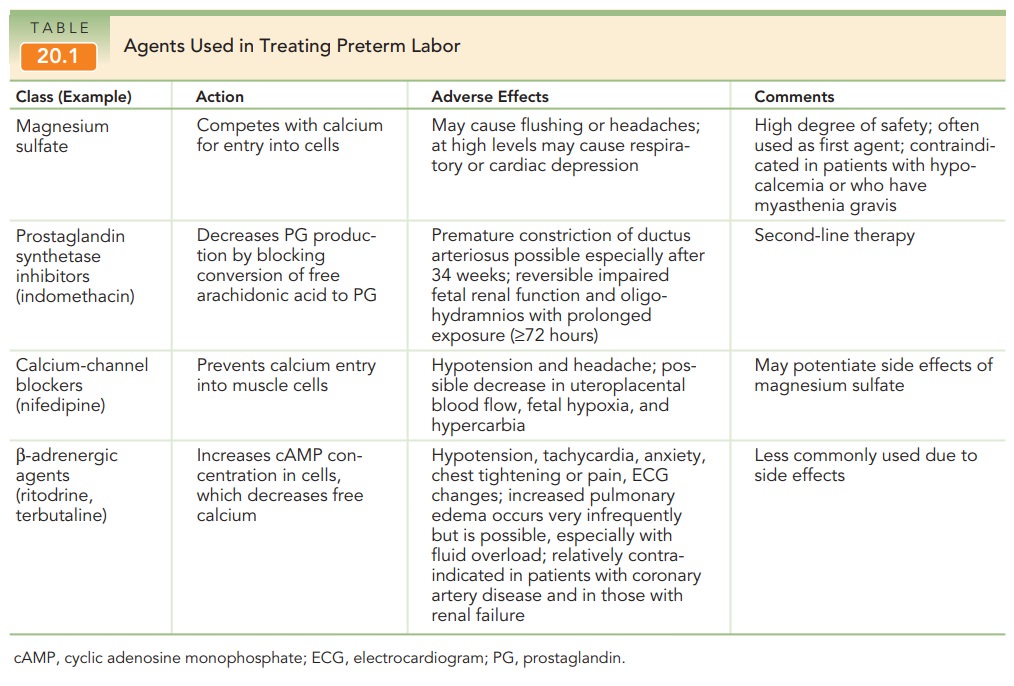
Various tocolytic therapies have
been used in the management of preterm labor (Table 20.1). Tocolytics have not
been shown to prolong pregnancy beyond sev-eral days (only 2 to 7). Different
treatment regimens ad-dress specific mechanisms involved in the maintenance of
uterine contractions, and each, therefore, may be best suited for certain
patients.
Typically,
patients with a diagnosis of preterm labor receive one form of tocolytic
therapy, with the addition or substitu-tion of other medications if the initial
treatment is considered unsuccessful.
Magnesium sulfate has been the
most frequently used agent, but use of nifedipine is increasing. Evidence as to
ef-ficacy beyond several days is weak, but often management allows for administration
of corticosteroid therapy. Adverse side effects, at times serious and even
life-threatening to the mother, can occur. The gestational age of the fetus is
always a consideration in deciding how vigorously to pur-sue therapy. For
example, maternal risks may be more ac-ceptable when treating a 26-week fetus
as compared to a 32-week fetus.
Contraindications to tocolysis include conditions in which the adverse effects of tocolysis may be significant, such as advanced labor, a mature fetus, a severely anom-alous fetus (from lethal congenital or chromosomal abnormalities), intrauterine infection, significant vaginal bleed-ing, and severe preeclampsia.
In addition,
a variety of obstetric complications, such as placental abruption, ad-vanced
cervical dilatation, or evidence of fetal compro-mise or placental
insufficiency, may contraindicate delay in delivery.
From 24 to 32 to 34 weeks of
gestation, management generally includes administration of corticosteroids (be-tamethasone or dexamethasone) to enhance fetal
pul-monary maturity. A single course of
corticosteroids should begiven to pregnant women between 24 and 32 weeks of
gestation who are at risk of preterm delivery. Both the incidence andseverity
of fetal respiratory distress syndrome are reduced with such therapy. Between
32 and 34 weeks of gestation,the use of steroids to enhance fetal lung maturity
is less certain. In addition, other sequelae of prematurity, such as
interventricular hemorrhage and necrotizing enterocoli-tis, occur less
frequently in infants whose mothers re-ceived corticosteroid therapy. Maximal
benefit to the fetus occurs if the therapy is administered within 7 days of
de-livery; however, routine weekly courses are not recom-mended because of
potential negative fetal effects.
Related Topics