Chapter: Obstetrics and Gynecology: Preterm Labor
Cause, Prediction, and Prevention of Preterm Labor
CAUSE, PREDICTION, AND PREVENTION OF PRETERM LABOR
Causes
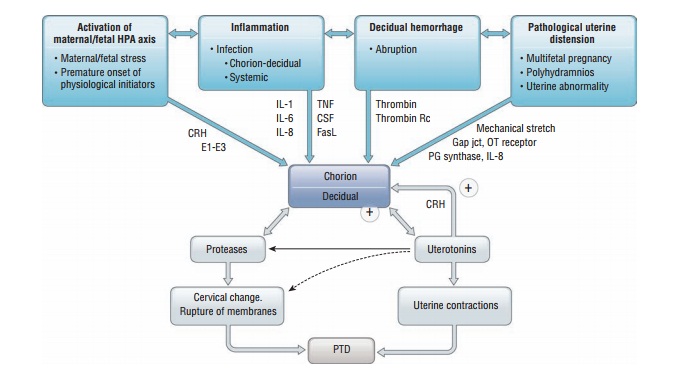
Preterm labor may represent a
final common pathway for a number of pathogenic processes. The four main
processes include: (1) activation of the maternal or fetal
hypothalamic-pituitary-adrenal axis due to maternal or fetal stress,
decidual-chorioamniotic or
systemic inflammation caused by infection, (3) decidual hemorrhage, or (4)
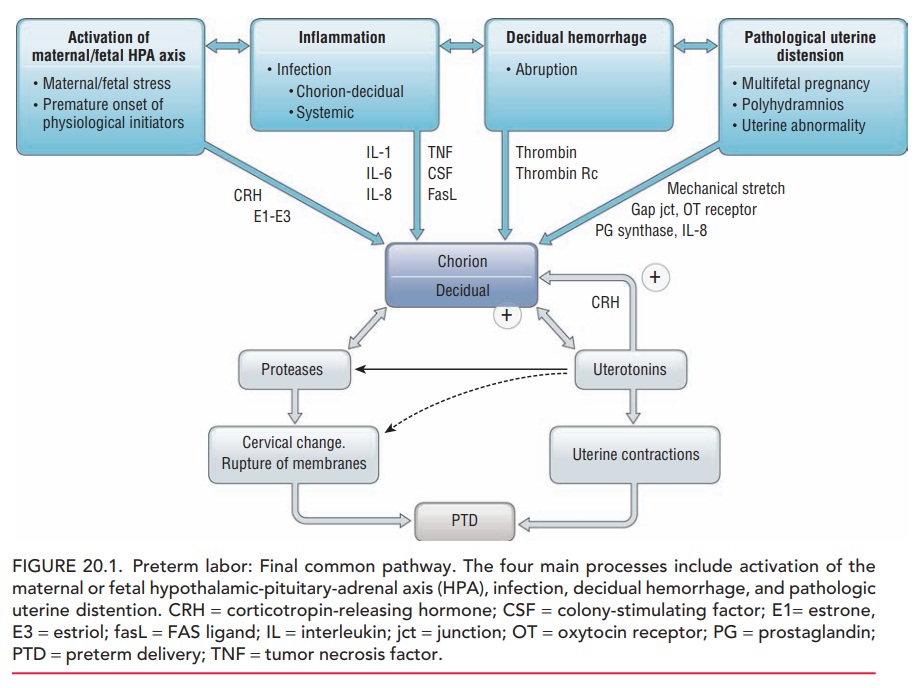
patho-logic uterine distention (Fig. 20.1). Numerous risk factors have been
associated with preterm labor (Box 20.1). Thestrongest
risk factor is multifetal gestation. With a priorpreterm birth, the risk in
a subsequent pregnancy increases and continues to increase with each subsequent
pregnancy. African-American women have higher rates of preterm birth associated
with preterm labor or preterm PROM, compared with other racial and ethnic
groups. Subclinical intra-amniotic infection has also been associated with
preterm labor and preterm PROM, especially when it oc-curs at earlier
gestational ages. In most cases, however,
no causeor risk factor for preterm labor can be identified.
Despite the lack of effective strategies to predict and prevent preterm labor, infant morbidity and mortality fol-lowing preterm birth have decreased over the last several decades as the result of several factors. First, neonatal in-tensive care management of preterm infants has greatly improved outcomes. Therefore, maternal transport to a regional tertiary-care center is indicated for women in preterm labor presenting to hospitals without sophisti-cated neonatal intensive care. Second, the use of cortico-steroids administered to a mother at immediate risk for preterm birth (such as a woman in preterm labor) has resulted in decreased incidence of respiratory distress syndrome, intraventricular hemorrhage, and associated infant morbidity and mortality.
Box 20.1
Factors Associated With Preterm Labor
Prior history of preterm birth
Preterm uterine contractions
Premature rupture of membranes (PROM)
African-American race
Cervical insufficiency
·
Primary
·
Secondary to surgery (e.g., cone biopsy of
cervix)
Infections
·
Urinary
·
Bacterial vaginosis
·
Intra-amniotic
Excessive uterine enlargement
·
Polyhydramnios
·
Multiple gestation
Uterine distortion
·
Leiomyomas
·
Septate uterus, uterine didelphys, and other
anomalies
Placental abnormalities
·
Placental abruption
·
Placenta previa
Maternal smoking (associated with PROM)
Iatrogenic: induction of labor
A major goal of therapy to stop contractions in a woman in preterm labor (tocolytictherapy) is to prolong pregnancy for up to 48 hours inorder to allow time to administer corticosteroids. Finally, prophylaxis against perinatal infection with group B strep-tococcus in women with preterm labor or preterm PROM has also decreased infant morbidity and mortality rates in the United States.
Prediction of Preterm Labor
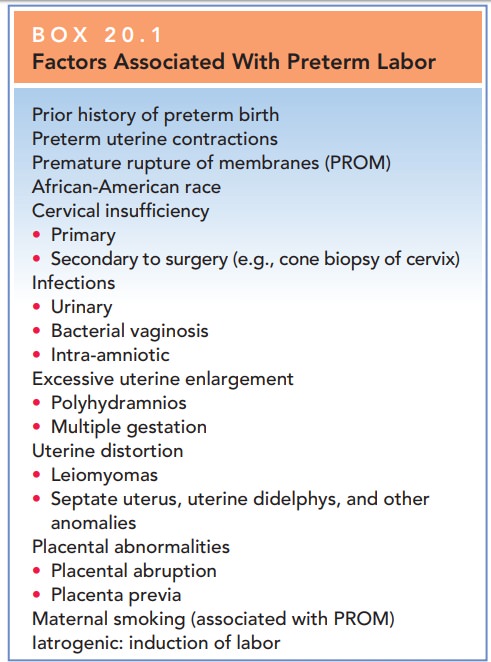
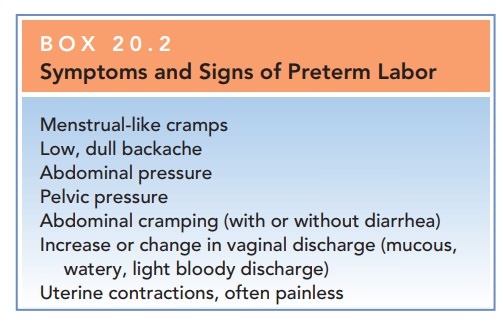
Patient and physician education
has focused on recogni-tion of the signs and symptoms that suggest preterm
labor (Box 20.2). Patients with symptoms are counseled to seek prompt medical
attention.
A number of factors are used to assess
signs and symp-toms and diagnose potential preterm labor. An increase in theconcentration of fetal
fibronectin( f FN) in cervicovaginal secre-tions is found with preterm
labor. Fetal fibronectin is an extra-cellular glycoprotein normally found
in the cervical mucus in early pregnancy and then again near term. A preterm
rise in the concentration of fFN may be associated with an in-creased
likelihood of birth between 22 and 34 weeks of ges-tation and birth within 7–14
days of the test. However, data combined from several studies reveal that the
positive pre-dictive value for delivery within a week is only 18%
Box 20.2
Symptoms and Signs of Preterm Labor
Menstrual-like cramps
Low, dull backache
Abdominal pressure
Pelvic pressure
Abdominal cramping (with or without diarrhea)
Increase or change in vaginal discharge (mucous,
watery, light bloody discharge)
Uterine contractions, often painless
The
greatest benefit of fFN appears to be its negative predictive value: if fFN is
absent (negative) in cervicovaginal secretions, the likelihood of delivery in
the next 7 days is very low.
Cervical length can also be used
as a diagnostic factor. As cervical
length decreases in midpregnancy, the risk for preterm birth has been shown to
increase in a continuous fash-ion. Transvaginal
ultrasoundexamination of the cervixis a reliable and reproducible method to
assess cervical length. This test may be most helpful when evaluating women at
high risk for recurrent preterm birth, those with uterine anomalies, and those
who have had prior cervical cone biopsy or multiple dilation and
curettage/evacuation procedures.
Early
asymptomatic dilation and effacement of the cervix (cervical insufficiency) may be associated with an increased
like-lihood of preterm labor and delivery. Interventions
such as pro-phylactic cervical cerclage on sonographic recognition of a
shortened cervical length (often defined as less than 2.5 cm) has not improved
outcomes.
Bacterial vaginosis (BV) is a common alteration ofthe vaginal flora that occurs in up to 40% of pregnant women and is associated with preterm labor and preterm PROM. BV diagnosed in symptomatic pregnant patients shouldthus be treated. Widespread screening and treatment forbacterial vaginosis in asymptomatic low-risk women and women with previous preterm birth has not been benefi-cial in decreasing the occurrence of preterm labor and is not recommended. Treatment for BV may be considered forwomen at high risk for preterm labor.
Prevention
There are
currently no uniformly effective interventions to prevent preterm labor,
regardless of risk factors. Prophy-lactic therapy—including
tocolytic drugs, bed rest, hydra-tion, and sedation in asymptomatic women at
high risk for preterm labor—has not been shown to be effective. However, in a
select group of women at very high risk who
have a documented history of
preterm birth, the use of weekly intramuscular injections of progesterone (17-α-hydroxyprogesterone caproate)
starting at 16–20 weeks of gestation and continuing until 36 weeks appears to
reduce spontaneous preterm birth. Vaginal progesterone supple-mentation in
women with an ultrasonically determined shortened cervical length has also
shown some benefit.
Related Topics