Chapter: Obstetrics and Gynecology: Third-Trimester Bleeding
Third-Trimester Bleeding: Placenta Previa
PLACENTA PREVIA
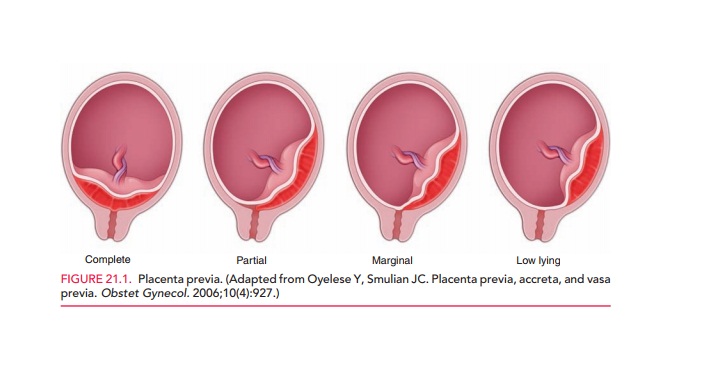
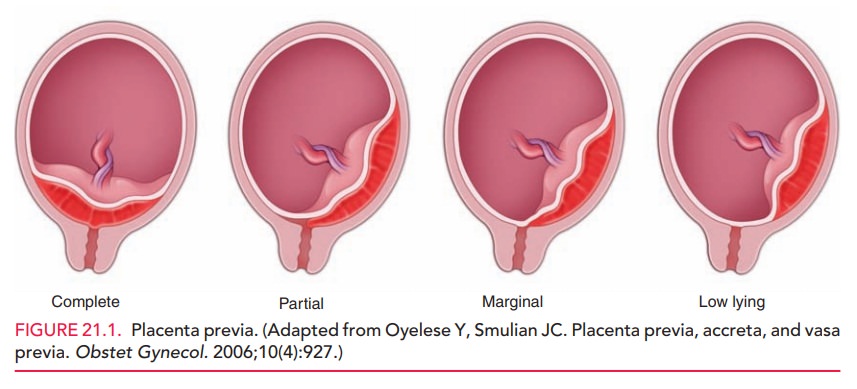
Placenta previa is a placental location close to
or over the inter-nal cervical os. It can be
classified ascomplete,in which
theplacenta completely covers the internal os, or partial, in which the placenta overlies part but not all of the
internal os. A placenta that extends into the lower uterine segment but does
not reach the internal os is called a low-lyingplacenta.
(Fig. 21.1.)
Placenta
previa classically presents with painless bleeding in the third trimester
In many cases there may be small
amounts of bleeding prior to a more significant episode of bleeding. About 75%
of women with placenta previa will have at least one episode of bleeding. On
average this episode occurs at around 29 to 30 weeks of gestation. In general,
placenta previa occurs in about 1 in 200 pregnancies. The incidence of placenta
pre-via earlier in pregnancy (approximately 24 weeks) is 4% to 5% and decreases
with increasing gestational age.
Complete placenta previa rarely
resolves sponta-neously, but partial and low-lying placenta previa will often
resolve by 32 to 35 weeks of gestation. The mech-anism does not involve an
upward “migration” of the placenta, but rather a stretching and thinning of the
lower uterine segment, which effectively moves the pla-centa away from the os.
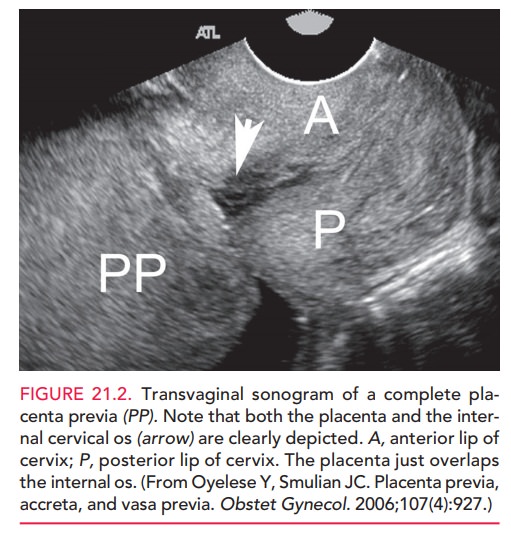
Transvaginal
ultrasonography is more accurate indiagnosing placenta previa than
abdominal ultrasonogra-phy, which gives many false-positive results,
particularly when the placenta is located posteriorly (Fig. 21.2). The etiology
of placenta previa is not known; however, it may be associated with abnormal
vascularization. Risk factors for
placenta previa include placenta previa in a prior preg-nancy (4% to 8%
recurrence), prior cesarean delivery or other uterine surgery, multiparity,
advanced maternal age, cocaine use, and smoking. Placenta previa has been
associ-ated with an increase in fetal anomalies, although the pre-cise
mechanism is unclear. These anomalies include severe cardiovascular, central
nervous system, gastrointestinal, and respiratory abnormalities.
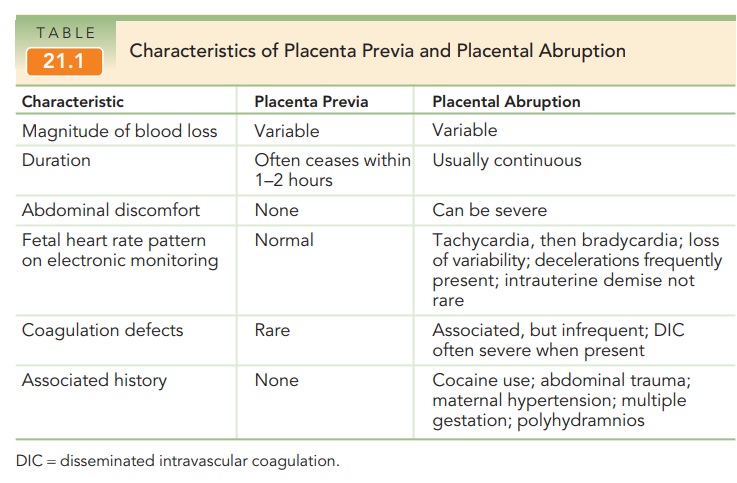
Bleeding usually ceases in 1 to 2 hours. Close observa-tion, fluid administration, bed rest, and administration of steroids for fetal lung maturity may be appropriate if the fetus is premature and the bleeding is not heavy enough to warrant immediate delivery. The bleeding is usually pain-less, except when it is associated with labor or abruption (the premature separation of the placenta; see Table 21.1 for a comparison of placenta previa and placental abrup-tion). For patients in a stable condition, outpatient managementmay be considered if the patient is compliant, lives close to the hos-pital, and has someone with her at all times. If the bleeding issevere or the fetus is at term, then delivery is appropriate.
Placenta previa is associated
with an increase in preterm birth and perinatal mortality and morbidity.
Delivery is most often via caesarean birth. In a patient whose condi-tion is
stable, caesarean delivery can be undertaken at 36 to 37 weeks of gestation,
following amniocentesis to confirm fetal lung maturity. If lung maturity is not
demonstrated, the patient should be delivered at 37 to 38 weeks of gestation.
Earlier caesarean delivery may be required if bleeding occurs or if the patient
goes into labor. The number of bleeding episodes is unrelated to the degree of
placenta previa or to fetal outcome.
Complications of placenta previa
also include increased bleeding from the lower uterine segment where the
pla-centa was attached at the time of cesarean delivery. The pla-centa may also
be abnormally adherent to the uterine wall. This is termed placenta accreta if the placental tissue extends into the
superficial layer of the myometrium, pla-centa
increta if it extends further into the myometrium, or placenta percreta if it extends completely through themyometrium
to the serosa, and sometimes into adjacent organs such as the bladder. The
incidence of placenta accreta is about 1 in 2500 deliveries, but increases in
patients with a history of cesarean delivery. The risk of requiring
hys-terectomy following a caesarean delivery for patients with placenta previa
is increased, which in turn increases the risk of maternal and perinatal
morbidity and mortality.
Related Topics