Chapter: Obstetrics and Gynecology: Third-Trimester Bleeding
Third-Trimester Bleeding: Placental Abruption
PLACENTAL ABRUPTION
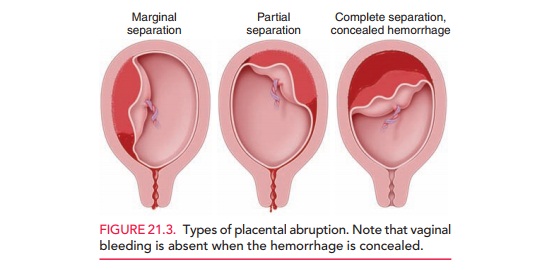
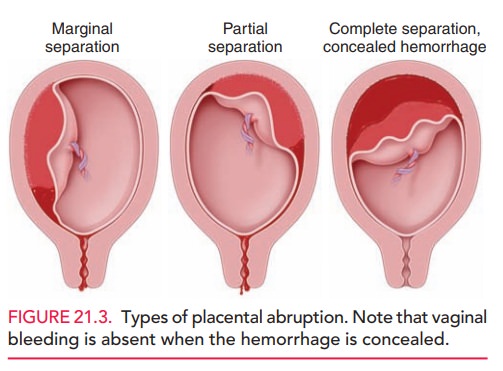
Placental abruption refers to an abnormal premature
separa-tion of an otherwise normally implanted placenta. There
arevarious types of abruption, depending upon the extent and region of
separation. A complete abruption
occurs when the entire placenta separates. A partial abruption exists when part of the placenta separates from
the uterine wall.
Marginal
abruption occurs when the separation is lim-ited to the edge
of the placenta (Fig. 21.3). A significant abruption requiring delivery occurs
in 1% of births.
Abruption occurs when bleeding in
the decidua basalis causes separation of the placenta and further bleeding. The
classic presentation of abruption is vaginal bleeding with abdominal pain.
Smaller or marginal abruptions may pre-sent with bleeding only. Concealed hemorrhage occurs when blood
is trapped behind the placenta and is unable to exit. Painful uterine
contractions, significant fetal heart rate abnormalities, and fetal demise may
occur in severe cases.
Risk factors for placental abruption include chronic hypertension, preeclampsia, multiple gestation, advanced maternal age, multiparity, smoking, cocaine use, preeclamp-sia, and chorioamnionitis. Trauma is also a major risk factor.
Abruption in a prior pregnancy
increases the risk of abrup-tion in subsequent pregnancy by 15- to 20-fold.
An
elevated second-trimester maternal serum alpha-fetoprotein (AFP) level may be
associated with up to a 10-fold increased risk of placental abruption due to
possible entry of AFP into the maternal circulation through the placental
uterine interface.
Abruption is often diagnosed by
clinical examination, although an ultrasound examination may be useful in less
severe cases not requiring immediate delivery. Abruption may occur in the
absence of ultrasound findings.
Management
of patients with placental abruptionincludes
monitoring of vital signs, fluid administration, and delivery for severe hemorrhage.
Expectant management may be appropriate for preterm patients with less severe
abruptions and minimal bleeding. Delivery is often by cesarean birth. Rarely,
blood penetrates the uterus to such an extent that the serosa becomes blue or
purple in color. This condition is called Couvelaire
uterus. A Kleihauer-Betke or similar test is essential to determine the
amount of fetal–maternal hemorrhage. Results guide decisions regarding
administration of Rh D immunoglobulin in women who are Rh D-negative and determine
the need for blood transfusion in the potentially anemic neonate. Coagulation
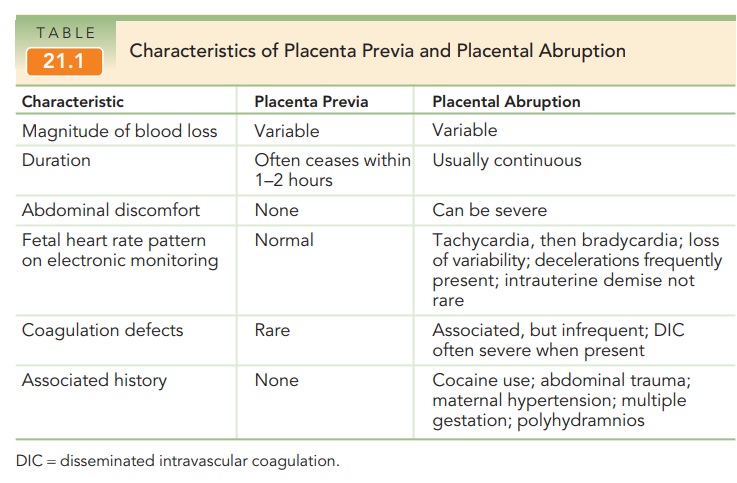
abnormalities may also be associated with abruption (see Table 21.1). Abruption
is the most com-mon cause of coagulopathy in pregnancy. Platelet counts may be
low and prothrombin time and partial thrombo-plastin time may be increased.
Serum fibrinogen may also be depleted. Disseminated intravascular coagulation
is a rare but extremely serious complication.
Related Topics