Chapter: Medical Physiology: Thyroid Metabolic Hormones
Synthesis and Secretion of the Thyroid Metabolic Hormones
Synthesis and Secretion of the Thyroid Metabolic Hormones
About 93 per cent of the metabolically active hormones secreted by the thyroid gland is thyroxine, and 7 per cent triiodothyronine. However, almost all the thy-roxine is eventually converted to triiodothyronine in the tissues, so that both are functionally important. The functions of these two hormones are qualita-tively the same, but they differ in rapidity and intensity of action. Triiodothy-ronine is about four times as potent as thyroxine, but it is present in the blood in much smaller quantities and persists for a much shorter time than does thyroxine.
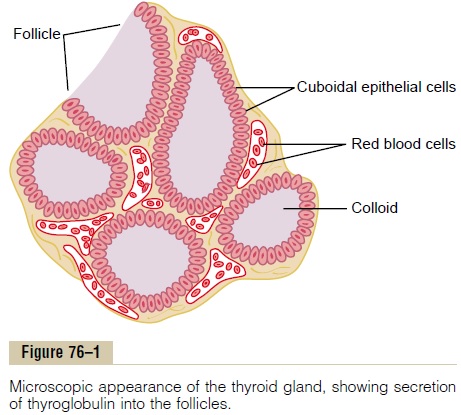
Physiologic Anatomy of the Thyroid Gland. The thyroid gland is composed, as shownin Figure 76–1, of large numbers of closed follicles (100 to 300 micrometers in diameter) filled with a secretory substance called colloid and lined with cuboidalepithelial cells that secrete into the interior of the follicles. The major constituentof colloid is the large glycoproteinthyroglobulin, which contains the thyroid hormones within its molecule. Once the secretion has entered the follicles, it must be absorbed back through the follicular epithelium into the blood before it can function in the body. The thyroid gland has a blood flow about five times the weight of the gland each minute, which is a blood supply as great as that of any other area of the body, with the possible exception of the adrenal cortex.
Iodine Is Required for Formation of Thyroxine
To form normal quantities of thyroxine, about 50 milligrams of ingested iodine in the form of iodides are required each year, or about 1 mg/week. To prevent iodine deficiency, common table salt is iodized with about 1 part sodium iodide to every 100,000 parts sodium chloride.
Fate of Ingested Iodides. Iodides ingested orally are absorbed from the gastro-intestinal tract into the blood in about the same manner as chlorides. Normally, most of the iodides are rapidly excreted by the kidneys, but only after about one fifth are selectively removed from the circulating blood by the cells of the thyroid gland and used for synthesis of the thyroid hormones.
Iodide Pump (Iodide Trapping)
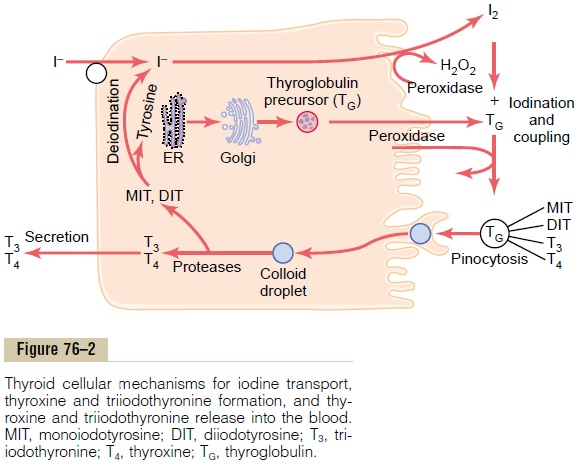
The first stage in the formation of thyroid hormones, shown in Figure 76–2, is transport of iodides from the blood into the thyroid glandular cells and follicles. The basal membrane of the thyroid cell has the specific ability to pump the iodide actively to the interior of the cell. This is called iodide trapping. In a normal gland, the iodide pump concentrates the iodide to about 30 times its concentration in the blood. When the thyroid gland becomes maximally active, this con-centration ratio can rise to as high as 250 times. The rate of iodide trapping by the thyroid is influenced by several factors, the most important being the concentration of TSH; TSH stimulates and hypophy-sectomy greatly diminishes the activity of the iodide pump in thyroid cells.
Thyroglobulin, and Chemistry of Thyroxine and Triiodothyronine Formation
Formation and Secretion of Thyroglobulin by the Thyroid Cells.
The thyroid cells are typical protein-secreting glandu-lar cells, as shown in Figure 76–2. The endoplasmic reticulum and Golgi apparatus synthesize and secrete into the follicles a large glycoprotein molecule called thyroglobulin, with a molecular weight of about335,000.
Each molecule of thyroglobulin contains about 70 tyrosine amino acids, and they are the major substrates that combine with iodine to form the thyroid hor-mones. Thus, the thyroid hormones form within the thyroglobulin molecule. That is, the thyroxine and triiodothyronine hormones formed from the tyrosine amino acids remain part of the thyroglobulin molecule during synthesis of the thyroid hormones and even afterward as stored hormones in the follicular colloid.
Oxidation of the Iodide Ion. The first essential step in theformation of the thyroid hormones is conversion of the iodide ions to an oxidized form of iodine, either nascent iodine (I0) or I3_, that is then capable of com-bining directly with the amino acid tyrosine. This oxi-dation of iodine is promoted by the enzyme peroxidase and its accompanying hydrogen peroxide, which provide a potent system capable of oxidizing iodides. The peroxidase is either located in the apical mem-brane of the cell or attached to it, thus providing the oxidized iodine at exactly the point in the cell where the thyroglobulin molecule issues forth from the Golgi apparatus and through the cell membrane into the stored thyroid gland colloid. When the peroxidase system is blocked or when it is hereditarily absent from the cells, the rate of formation of thyroid hor-mones falls to zero.
Iodination of Tyrosine and Formation of the Thyroid Hormones— “Organification” of Thyroglobulin. The binding of iodinewith the thyroglobulin molecule is called organifica-tion of the thyroglobulin. Oxidized iodine even in themolecular form will bind directly but very slowly with the amino acid tyrosine. In the thyroid cells, however, the oxidized iodine is associated with an iodinase enzyme (Figure 76–2) that causes the process to occur within seconds or minutes.Therefore, almost as rapidly as the thyroglobulin molecule is released from the Golgi apparatus or as it is secreted through the apical cell membrane into the follicle, iodine binds with about one sixth of the tyrosine amino acids within the thyroglobulin molecule.
Figure 76–3 shows the successive stages of iodination of tyrosine and final formation of the two important thyroid hormones, thyroxine and tri-iodothyronine. Tyrosine is first iodized to monoiodoty-rosine and then to diiodotyrosine. Then, during thenext few minutes, hours, and even days, more and more of the iodotyrosine residues become coupled with one another.
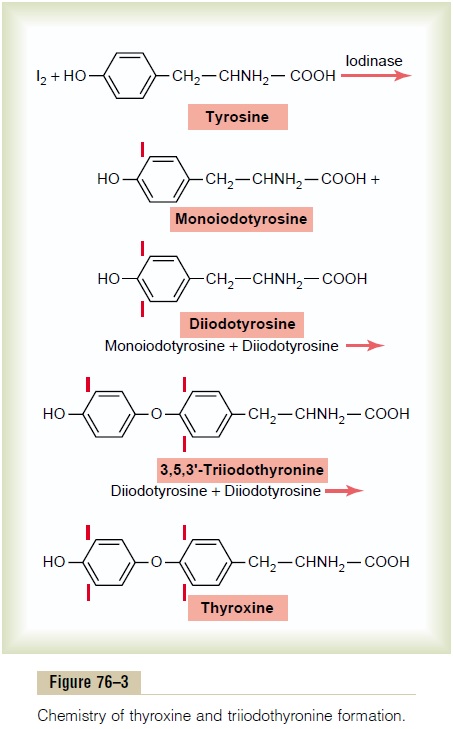
The major hormonal product of the coupling reaction is the molecule thyroxine that remains part of the thyroglobulin molecule. Or one molecule of monoiodotyrosine couples with one molecule of diiodotyrosine to form triiodothyronine, which repre-sents about one fifteenth of the final hormones.
Storage of Thyroglobulin. The thyroid gland is unusualamong the endocrine glands in its ability to store large amounts of hormone. After synthesis of the thyroid hormones has run its course, each thyroglobulin mol-ecule contains up to 30 thyroxine molecules and a few triiodothyronine molecules. In this form, the thyroid hormones are stored in the follicles in an amount suf-ficient to supply the body with its normal requirements of thyroid hormones for 2 to 3 months. Therefore, when synthesis of thyroid hormone ceases, the physi-ologic effects of deficiency are not observed for several months.
Release of Thyroxine andTriiodothyronine from theThyroid Gland
Thyroglobulin itself is not released into the circulating blood in measurable amounts; instead, thyroxine and triiodothyronine must first be cleaved from the thy-roglobulin molecule, and then these free hormones are released. This process occurs as follows: The apical surface of the thyroid cells sends out pseudopod exten-sions that close around small portions of the colloid to form pinocytic vesicles that enter the apex of the thyroid cell. Then lysosomes in the cell cytoplasm immediately fuse with these vesicles to form digestive vesicles containing digestive enzymes from the lyso-somes mixed with the colloid. Multiple proteases among the enzymes digest the thyroglobulin mole-cules and release thyroxine and triiodothyronine in free form. These then diffuse through the base of the thyroid cell into the surrounding capillaries. Thus, the thyroid hormones are released into the blood.
About three quarters of the iodinated tyrosine in the thyroglobulin never becomes thyroid hormones but remains monoiodotyrosine and diiodotyrosine.
During the digestion of the thyroglobulin molecule to cause release of thyroxine and triiodothyronine, these iodinated tyrosines also are freed from the thyroglob-ulin molecules. However, they are not secreted into the blood. Instead, their iodine is cleaved from them by a deiodinase enzyme that makes virtually all this iodineavailable again for recycling within the gland for forming additional thyroid hormones. In the congeni-tal absence of this deiodinase enzyme, many persons become iodine-deficient because of failure of this recy-cling process.
Daily Rate of Secretion of Thyroxine and Triiodothyronine.
About 93 per cent of the thyroid hormone released from the thyroid gland is normally thyroxine and only 7 per cent is triiodothyronine. However, during the ensuing few days, about one half of the thyroxine is slowly deiodinated to form additional triiodothyro-nine. Therefore, the hormone finally delivered to and used by the tissues is mainly triiodothyronine, a total of about 35 micrograms of triiodothyronine per day.
Transport of Thyroxine and Triiodothyronine to Tissues
Thyroxine and Triiodothyronine Are Bound to Plasma Proteins.
On entering the blood, over 99 per cent of the thy-roxine and triiodothyronine combines immediately with several of the plasma proteins, all of which are synthesized by the liver. They combine mainly with thyroxine-binding globulin and much less so with thyroxine-binding prealbumin and albumin.
Thyroxine and Triiodothyronine Are Released Slowly to Tissue Cells. Because of high affinity of the plasma-bindingproteins for the thyroid hormones, these substances— in particular, thyroxine—are released to the tissue cells slowly. Half the thyroxine in the blood is released to the tissue cells about every 6 days, whereas half the triiodothyronine—because of its lower affinity—is released to the cells in about 1 day.
On entering the tissue cells, both thyroxine and tri-iodothyronine again bind with intracellular proteins, the thyroxine binding more strongly than the tri-iodothyronine. Therefore, they are again stored, but this time in the target cells themselves, and they are used slowly over a period of days or weeks.
Thyroid Hormones Have Slow Onset and Long Duration of Action.
After injection of a large quantity of thyroxine into a human being, essentially no effect on the metabolic rate can be discerned for 2 to 3 days, thereby demon-strating that there is along latent period before thy-roxine activity begins. Once activity does begin, it increases progressively and reaches a maximum in 10 to 12 days, as shown in Figure 76–4. Thereafter, it decreases with a half-life of about 15 days. Some of the activity persists for as long as 6 weeks to 2 months.
The actions of triiodothyronine occur about four times as rapidly as those of thyroxine, with a latent
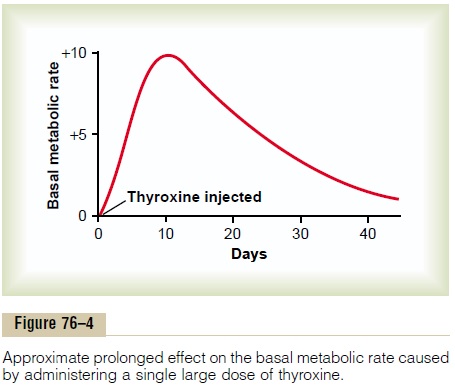
Most of the latency and prolonged period of action of these hormones are probably caused by their binding with proteins both in the plasma and in the tissue cells, followed by their slow release. However, we shall see in subsequent discussions that part of the latent period also results from the manner in which these hormones perform their functions in the cells themselves.
Related Topics