Chapter: Essentials of Psychiatry: Clinical Evaluation and Treatment Planning: A Multimodal Approach
Psychiatric Interview
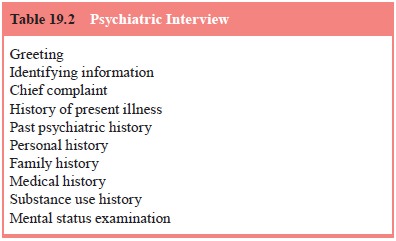
Psychiatric Interview
Despite the advent of brain imaging tests,
standardized diag-nostic criteria and structured rating scales, the psychiatric
inter-view (Table 19.2) remains the cornerstone of clinical evaluation in
psychiatry. Whether it is conducted in a busy psychiatric emer-gency room, an
inpatient ward, or an outpatient office, the psy-chiatric interview is
essential for establishing rapport with the patient, initiating the therapeutic
alliance, eliciting the psychiat-ric history and performing the Mental Status
Examination. When conducted skillfully, the interview may appear to be a
relaxed and casual conversation, but it is actually an extremely precise
diagnostic tool composed of specific elements: the identifying in-formation,
the chief complaint, the history of present illness, the past psychiatric
history, the personal history, the family history, the medical history, the
substance use history and the Mental Status Examination (MSE). The essential
features of the psychi-atric interview are highlighted here.
Before beginning, the psychiatrist should introduce
him-self or herself, explain the purpose of the interview, and try to make the
patient as comfortable as possible. The interview gives the most accurate
information when the psychiatrist and patient speak in a language in which they
are both fluent. When this is not possible, a translator should be used,
preferably one with mental health training or experience. Even then, some of
the sub-tleties of the patient’s communications are lost.
Identifying Information
Most interviewers find it helpful to begin with a
few questions designed to identify the patient in a general way. Asking the
pa-tient’s name, age, address, marital status and occupation provides a quick
general picture and begins the interview with emotion-ally neutral material. If
the interviewer chooses to begin in this way, it is important to complete this
section rapidly and then give the patient a chance to respond to open-ended
questions. This al-lows the interviewer to gain a more accurate sense of the
patient’s spontaneous speech patterns, thought processes and thought con-tent.
If the patient becomes too disorganized in response to this change, the
psychiatrist can revert to more focused questions to structure and organize the
interview. If it is possible, within the context of the interview, other pieces
of identifying information, such as the patient’s ethnic group and religious
affiliation, should be obtained.
Chief Complaint
At the start, the interviewer wants to ascertain
exactly why the pa-tient is seeking psychiatric help at this time. The
interviewer may begin with a fairly general question, such as “What brings you
to treatment at this time?’’ The patient may have a long history of psychiatric
illness, but the chief complaint refers only to the acute problem that
necessitates the current intervention. The in-terviewer should try to help the
patient distinguish the chief com-plaint from any chronic problems, as in the
following example:
Interviewer: Can you
tell me what brings you to see a psychiatrist at this time?
Patient: Well, I
have had schizophrenia for 25 years.
Interviewer: I see.
But my guess is that something happened re-cently that has prompted you to come
in today, rather than several months ago.
Patient: Oh, yes.
Yesterday my wife kicked me out of the house.
I’m homeless.
Here the patient’s chief complaint is homelessness;
the schizophre-nia is part of his psychiatric history. Although a psychotic
patient may offer a chief complaint that seems incoherent or unrealistic, it is
important to collect the chief complaint in the patient’s words and later look
to other sources of information for additional his-tory. Similarly, in response
to the question, “What brings you to seek psychotherapy at this time?’’ a
patient may begin to answer by detailing his or her childhood, but the
interviewer should help the patient to focus on current issues that
precipitated the consul-tation. Some patients may not be able to cite a chief
complaint: “My wife sent me’’ or “There’s no problem. I don’t know why the
police picked me up’’. Even these answers give the interviewer information
about the patient’s current situation, which can be elaborated on by asking the
patient for more details.
When the interview is being conducted for a third
party – for example to determine whether a patient is eligible for dis-ability
– the chief complaint is replaced by the purpose of the interview. The
psychiatrist should review such purpose with the patient and discuss the limits
of confidentiality.
History of Present Illness
Having obtained the chief complaint, the
interviewer should clarify the nature of the present illness. By definition,
the present illness begins with the onset of signs and symptoms that
char-acterize the current episode of illness. For example, the present illness
of a manic patient with chronic bipolar disorder who was asymptomatic for the
past 3 years would begin with the onset of the current episode of mania. The
interviewer should determine the duration of the present illness, as well as precipitating
fac-tors such as psychosocial stressors, substance use, discontinuing
medication and medical illnesses. The patient should be allowed to tell the
story, and the clinician should follow-up with specific diagnostic questions.
For example, a patient who tells a story of 6 months of sadness after the death
of a relative should then be asked about vegetative symptoms of depression,
suicidal ideation and guilty rumination.
Past Psychiatric History
The interviewer should ask for information regarding any previ-ous episodes of psychiatric illness or treatment, including hospi-talization, medications, outpatient therapy, substance use treat-ment, self-help groups and consultation with culture-specific healers such as shamans. The duration and effectiveness of treat-ment should be ascertained, as well as the patient’s general expe-rience of her or his psychiatric treatment to date.
Personal History
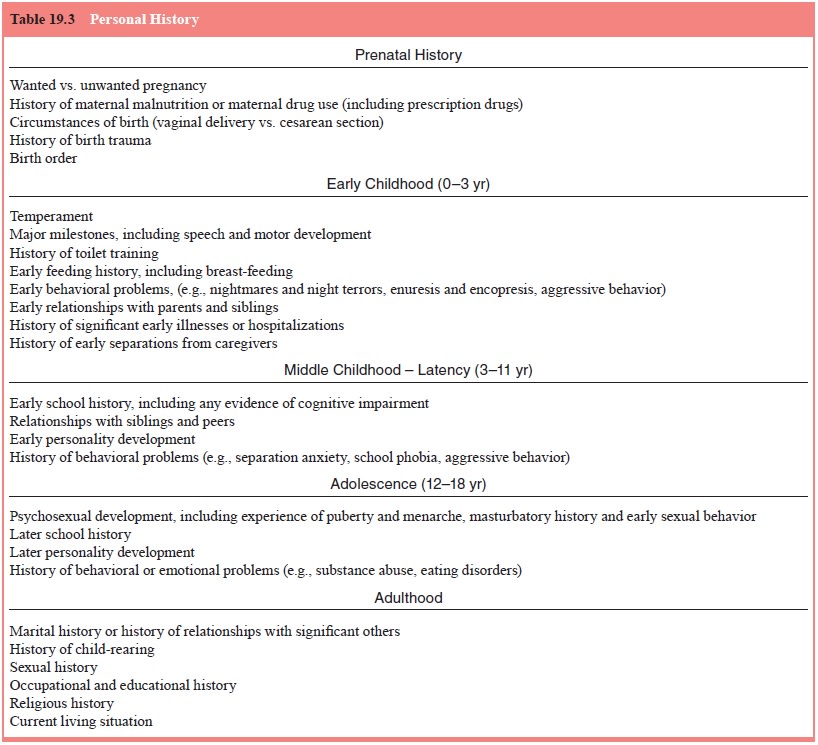
No interview is complete without some understanding
of the pa-tient’s background and life circumstances (Table 19.3). Within the
constraints of the interviewer’s time and the patient’s toler-ance for further
questioning, the clinician should inquire about the patient’s upbringing,
educational and vocational history, in-terpersonal relations and current social
situation. It is important to inquire about the patient’s sexual history and to
ask about risk factors for human immunodeficiency virus (HIV) infection, such
as a history of multiple partners, unprotected vaginal and anal in-tercourse,
and intravenous drug use. This information is relevant not only for the
assessment and diagnosis of the present illness but also for treatment
planning.
Family History
The interviewer should ask the patient specifically
about any relatives with a history of psychiatric illness or treatment,
sui-cide, or substance use. This information may be of diagnostic importance.
For example, a patient who presents with a firstepisode of acute psychosis may
have any one of a number of dis-orders, but a family history of affective
disorders may lead the interviewer to suspect a diagnosis of bipolar disorder
or major depression with psychotic features rather than schizophrenia. This
information is also important for treatment planning, par-ticularly if the
patient’s primary caregivers are also psychiatri-cally ill or also abuse
substances.
Medical History
A careful review of a patient’s medical history is
an important part of the psychiatric interview because medical conditions can
dramatically affect psychiatric status. Many medical disorders such as
endocrinological conditions (thyroid disease, pheochro-mocytomas, pituitary
adenomas), neurological disorders (Par-kinson’s disease, central nervous system
neoplasms, Wilson’s disease, stroke syndromes, head trauma) and infectious
diseases (HIV infection, meningitis, sepsis) can have manifestations that
include psychiatric symptoms. When such a disorder is suspected, rigorous
inquiry is essential. A review of all of the patient’s medications, including
over-the-counter preparations and alternative remedies, is important because
many of these substances can produce or exacerbate psychiatric symptoms. For
example, propranolol taken for hypertension may produce symptoms of depression,
and scopolamine taken for mo-tion sickness may induce delirium. Finally, the
toll of chronic, de-bilitating medical conditions or the acute onset of a
catastrophic physical illness may be accompanied by secondary psychiatric
symptoms that can be fully understood only in the context of the patient’s medical
condition.
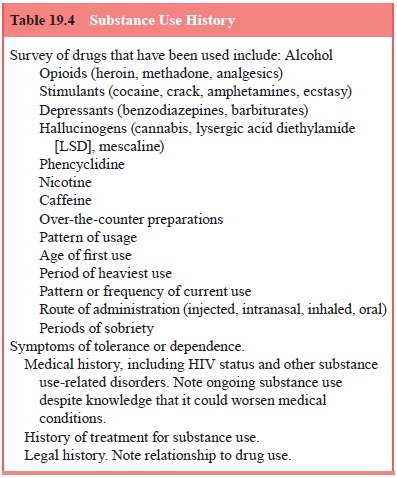
Substance Use History
The interviewer should inquire about which
substances are used, under what circumstances, and the quantity, variety, and
duration of use (Table 19.4). A question such as “Do you drink alcohol?’’ is
likely to be answered with a quick “No’’. A better question, such as “How much
alcohol do you drink?’’ communicates to the pa-tient that the clinician is not
making a value judgment and is more likely to elicit an accurate answer. The
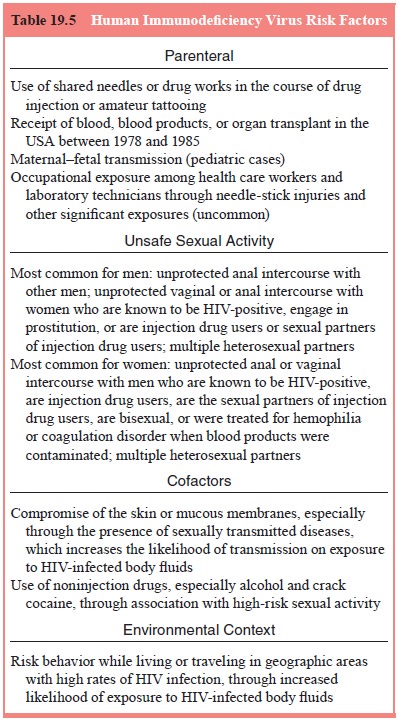
interviewer must be sure to ask about past and current drug injection,
including the sharing of injection equipment, to assess for HIV risk factors
(Table 19.5).
Mental Status Examination
The MSE is a structured way to assess a patient’s
mental state at a given time. Unlike the parts of the interview that focus on
the history, the MSE provides a descriptive snapshot of the patient at the
interview. Much of the information needed for the evaluation of appearance,
behavior and speech is gathered without specific questioning during the course
of the interview. However, the interviewer generally wants to ask specific
questions to assess the patient’s mood, thought process and content and
cognitive functioning. Bearing in mind the outline of the MSE (Table 19.6)
ensures that the interview is comprehensive. The components of the MSE are
described in the following paragraphs.
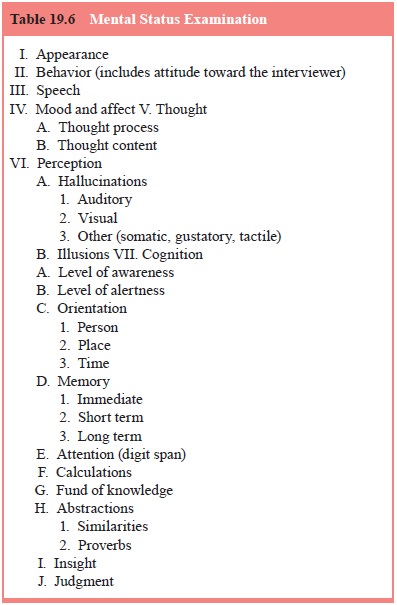
Appearance
The interviewer should note the patient’s general
appearance, in-cluding grooming, level of hygiene and attire.
Behavior
This includes patient’s level of cooperativeness
with the inter-view, motor excitement or retardation, abnormal movements (e.g.,
tardive dyskinesia, tremors), and maintenance of eye con-tact with the
interviewer.
Speech
The psychiatrist should carefully assess the patient’s speech for rate, fluency, clarity and softness or loudness. The interviewer may want to question the patient directly about his or her speech. For example, the psychiatrist can gain valuable diagnostic informa-tion by asking a patient with pressured speech if she or he is able to modulate the rate of the speech or by asking whether a dysarthric patient is aware of not speaking clearly. A bipolar patient who is in the midst of a manic episode is not able to slow down her or his speech; a fast-talking anxious person is able to do so. Similarly a patient whose dysarthria is secondary to ill-fitting dentures is aware of this problem whereas an intoxicated person is not. It is helpful to clarify whether patients with a speech abnormality feel that this is their normal speech pattern or a new problem.
Mood and Affect
The interviewer should be aware of the patient’s
mood and affect. This may be evident from the way in which the patient answers
other questions and tells the history, but specific questions are often
indicated. The patient’s mood is a pervasive affective state, and it is often
helpful simply to ask, “What has your mood been like lately?’’ or “How would
you describe your mood?’’ In con-trast, affect is the way in which one
modulates and conveys one’s feeling state from moment to moment. The clinician
judges the congruity between the material the patient is presenting and the
accompanying affect, that is, sadness when discussing the death of a loved one
or happiness when describing a child’s accom-plishments. This reveals whether
the affect is labile (shifts too rapidly) and whether it is appropriate to the
content of the mate-rial.
Thought
The clinician should assess the patient’s thought
process and con-tent. Thought process is the form of the patient’s thoughts –
are they organized and goal directed or are they tangential, circum-stantial,
or loosely associated? If the patient’s thought processes are difficult to
understand, the clinician can indicate his or her difficulty in fol-lowing what
is being said and then assess the patient’s response to this intervention. Some
patients – such as patients with stroke who have nonfluent aphasias – may
appear to have disorganized speech but are aware that they are not making
sense, whereas those with fluent aphasias, psychosis and delirium are not
nec-essarily aware of their impairment. The psychiatrist should ask
specifically about the patient’s thought content, including delu-sions
(grandiose, persecutory, somatic), hallucinations (auditory, visual, tactile
and olfactory), obsessions, phobias, and suicidal and homicidal ideation.
Although these questions should be asked with tact and empathy, they should
always be asked. Pa-tients are generally relieved that the interviewer has
broached the subject of suicide, and simply asking the question does not give
patients ideas they have not had before.
Cognition
Every psychiatric interview should include some
assessment of the patient’s cognitive functioning. This includes the patient’s
level of awareness, alertness and orienta-tion (to person, place and time). If
there is a question about the patient’s memory, formal memory testing may be
done to assess short-term, intermediate and long-term memory. A patient who can
answer questions for 30 minutes is clearly attentive, but any doubts about the
patient’s attentiveness should prompt a formal assessment, for example, asking
the patient to recite a series of digits forward and backward. Before assessing
the patient’s cal-culations and fund of knowledge, it is important to ascertain
the patient’s level of education. Formal assessment of the patient’s ability to
abstract may be unnecessary for a patient who has used abstract constructions
throughout the interview, but the inter-viewer may want to ask formally for interpretations
of similes and proverbs. It is often helpful to begin with simple
constructions, for example, asking the patient the meaning of such phrases as
“He has a warm heart’’ or “Save your money for a rainy day’’. Patients whose
native language is not English may have difficulty in this area that does not
reflect a lack of ability to abstract.
The interviewer should gain a full understanding of
the pa-tient’s insight into the illness by asking why, in the patient’s
opin-ion, he/she is currently in need of psychiatric care and what has caused
problems. Finally, the interviewer should learn about the patient’s judgment.
This is best assessed in terms of the circum-stances of the patient’s life, for
example, asking a mother how she would deal with a situation in which she had
to leave her children to go to the store or asking a chronically ill person
what he does when he sees that he is running out of medicine.
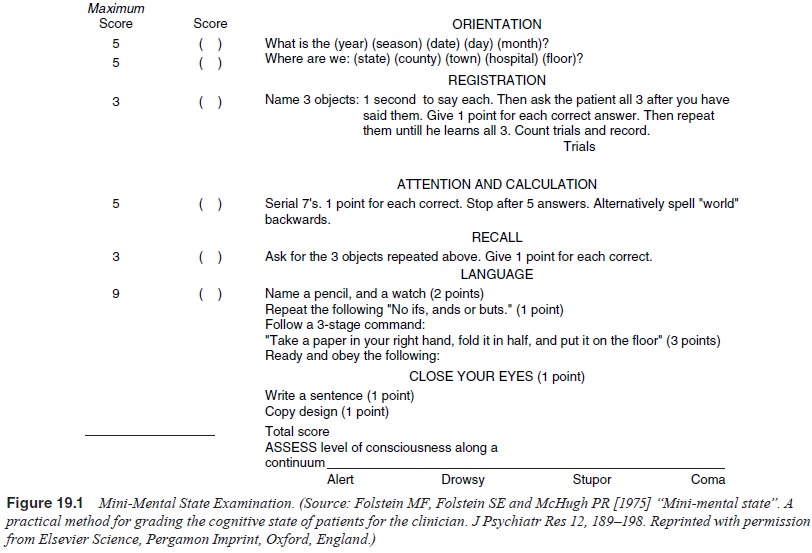
The interviewer may want to use the Mini-Mental
State Examination (Mini-MSE) to quantify the degree of cognitive im-pairment of
a patient with obvious cognitive abnormalities. This can be useful as an
initial diagnostic tool, as well as a means of assessing changes in cognitive
function over time. The Mini-MSE is outlined in Figure 19.1.
Related Topics