Chapter: Basic & Clinical Pharmacology : Vasodilators & the Treatment of Angina Pectoris
Pathophysiology of Angina
PATHOPHYSIOLOGY OF ANGINA
Determinants of Myocardial Oxygen Demand
The
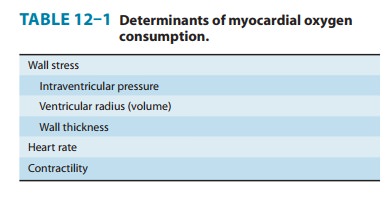
major determinants of myocardial oxygen requirement are set forth in Table
12–1. The effect of arterial blood pressure is medi-ated through its effect on
wall stress. As a consequence of its continuous activity, the heart’s oxygen
needs are relatively high, and it extracts approximately 75% of the available
oxygen even in the absence of stress. The myocardial oxygen requirement
increases when there is an increase in heart rate, contractility, arterial
pres-sure, or ventricular volume. These hemodynamic alterations fre-quently
occur during physical exercise and sympathetic discharge, which often
precipitate angina in patients with obstructive coro-nary artery disease.
Drugs that reduce cardiac size, rate, or force reduce cardiac oxygen demand. Thus, vasodilators, β blockers, and calcium block-ers have predictable benefits in angina. A small, late component of sodium current helps to maintain the long plateau and prolong the calcium current of myocardial action potentials. Drugs that block this late sodium current can indirectly reduce calcium influx and consequently reduce cardiac contractile force. The heart favors fatty acids as a substrate for energy production. However, oxidation of fatty acids requires more oxygen per unit of ATP generated than oxidation of carbohydrates. Therefore, drugs that shift myocardial metabolism toward greater use of glucose (fatty acid oxidation inhibitors) have the potential, at least in theory, to reduce the oxy-gen demand without altering hemodynamics.
Determinants of Coronary Blood Flow & Myocardial Oxygen Supply
Increased
demand for oxygen in the normal heart is met by aug-menting coronary blood
flow. Coronary blood flow is directly related to the perfusion pressure (aortic
diastolic pressure) and the duration of diastole. Because coronary flow drops
to negligible values during systole, the duration of diastole becomes a
limiting factor for myocardial perfusion during tachycardia. Coronary blood
flow is inversely proportional to coronary vascular resis-tance. Resistance is
determined mainly by intrinsic factors— including metabolic products and
autonomic activity—and by various pharmacologic agents. Damage to the
endothelium of coronary vessels has been shown to alter their ability to dilate
and to increase coronary vascular resistance.
Determinants of Vascular Tone
Peripheral
arteriolar and venous tone (smooth muscle tension) both play a role in
determining myocardial wall stress (Table 12–1). Arteriolar tone directly
controls peripheral vascular resistance and thus arterial blood pressure. In
systole, intraventricular pressure must exceed aortic pressure to eject blood;
arterial blood pressure thus determines the systolic
wall stress in an important way. Venous tone determines the capacity of the
venous circulation and con-trols the amount of blood sequestered in the venous
system versus the amount returned to the heart. Venous tone thereby determines
the diastolic wall stress.
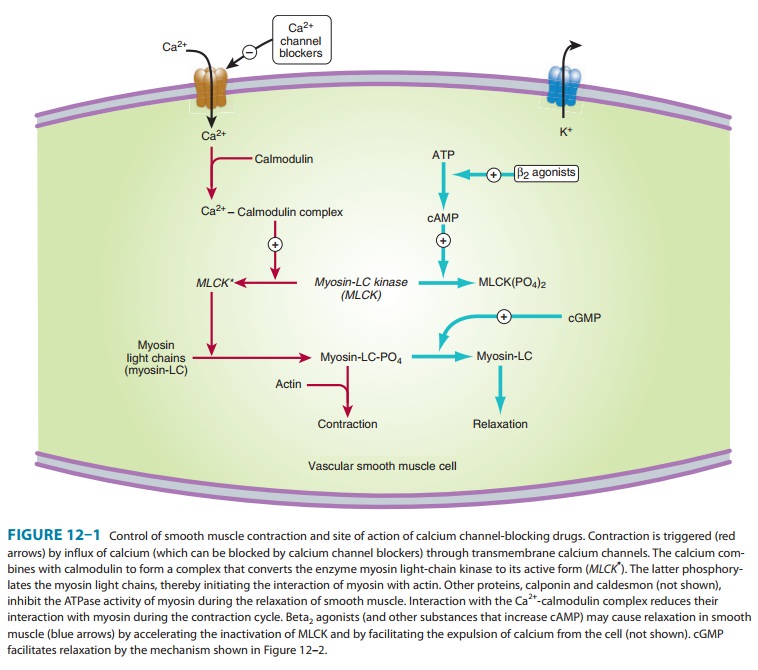
The
regulation of smooth muscle contraction and relaxation is shown schematically
in Figure 12–1. The mechanisms of action of the major types of vasodilators are
listed in Table 11–2. As shown in Figures 12–1 and 12–2, drugs may relax
vascular smooth muscle in several ways:
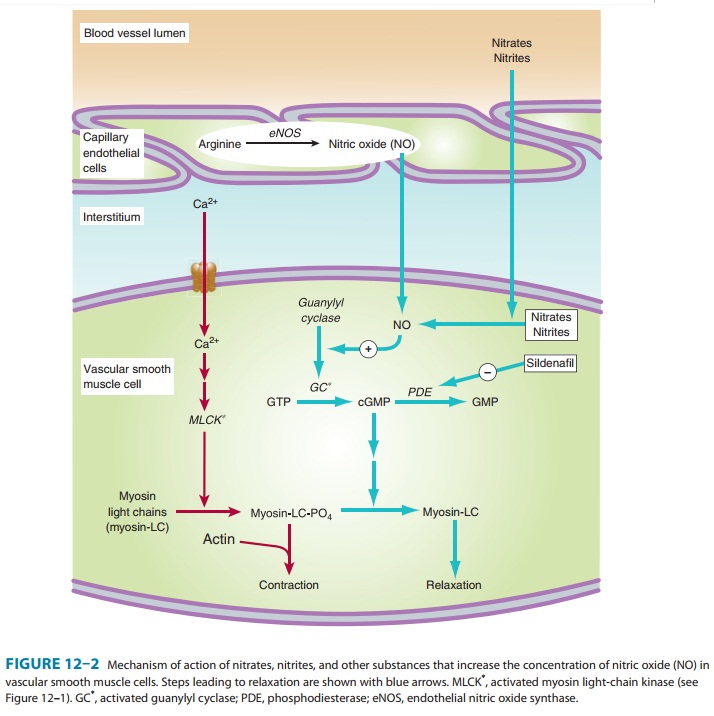
1.
Increasing cGMP: As indicated in
Figures 12–1 and 12–2,cGMP facilitates the dephosphorylation of myosin light
chains, preventing the interaction of myosin with actin. Nitricoxide is an effective activator of soluble guanylyl cyclase
andacts mainly through this mechanism. Important molecular donors of nitric
oxide include nitroprusside and the organic nitrates used in angina.
2.
Decreasing
intracellular Ca2+: Calcium channel blockers predictably cause vasodilation
because they reduce intracel-lular Ca2+, a major modulator of the
activation of myosin light chain kinase (Figure 12–1). Beta blockers and calciumchannel
blockers also reduce Ca2+influx in cardiac musclefibers, thereby
reducing rate, contractility, and oxygen require-ment under most circumstances.
3.
Stabilizing or
preventing depolarization of the vascular smooth muscle cell membrane: The membrane potential
ofexcitable cells is stabilized near the resting potential by increas-ing
potassium permeability. Potassium channel openers, such as minoxidil
sulfate increase the permeability of K+
channels, probably ATP-dependent K+ channels. Certain newer agents
under investigation for use in angina (eg, nic-orandil)
may act, in part, by this mechanism.
4. Increasing cAMP in vascular smooth muscle cells: As shownin Figure 12–1, an increase in cAMP increases the rate of inac-tivation of myosin light chain kinase, the enzyme responsible for triggering the interaction of actin with myosin in these cells. This appears to be the mechanism of vasodilation caused by β2 agonists, drugs that are not used in angina (because they cause too much cardiac stimulation), and by fenoldopam, a D1 agonist used in hypertensive emergencies.
Related Topics